WingRight
End of life
Front lines in the ICU with COVID-19
Reality is teaching a hard reality lesson with COVID-19.
This video concerns the minority of COVID-19 patients who require intensive care and the less than 1 percent who die of the disease. The discussion about the course of the disease and treatment is possibly too technical and brutal for the general public, so watch the whole thing with care.
However, I’m hoping to spur conversations about end of life in light of the broader COVID-19 crisis and specific crisis events.
This is a tough, highly technical discussion between Dr. Zubin Damania, a blogger otherwise known as “ZDoggMD” and Barbara McClean, MN, RN, CCRN, NP-PC, an expert in Critical Care & Intensive Care medicine in an Atlanta, Georgia teaching hospital with over 100 ICU beds. The first few minutes show Barbara McClean as a compassionate caring practitioner and educator. I believe and trust what she says about the worst case (stressing, again: fortunately these are the minority!) outcomes with COVID-19.
If you want to get to the meat of the video, there’s a “philosophical discussion” about the very real, unique in this modern age, futility of CPR in COVID-19 patients whose hearts stop due to the disease at 35:00 to 41:00.
There’s also interesting information about Personal Protective Equipment (PPE) difficulty (not shortage, but the physical reality) at the segment 30:00 to 35:00 minutes.
COVID-19 is, as Ms. McLean says, an unpredictable, sometimes deadly disease. Currently, patients can go from minor symptoms to death due to respiratory failure and cardiac arrest in as little as 4 hours. There is very little success to date in attempts to resuscitate patients who “code,” whose hearts stop, while in distress due to the virus.
I can’t stress enough that we need to talk, we need to make decisions among our families and to understand that this disease takes some options, some autonomy we have come to assume are our rightful “choices,” completely off the table. This disease doesn’t care what we want.
I’m unable to turn comments back on for this post. Please post comments to my Facebook page and I will try to keep up with replies. Let’s keep this on the level of philosophy and medical ethics. I will delete political criticisms.
Let’s keep this on the level of philosophy and medical ethics. I will delete political criticisms.
To kill or not to kill – or even to call it killing?
It seems that an advocate of Euthanasia and Assisted Suicide (EAS), which is legal in Canada since 2016, complained to the “The Protection of Conscience Project” administrators about their use of the word, “killing,” rather than “Medically Assisted Death” (MAD) when writing about the law. The wording of the objection exposes the potential limitations even on thoughts, much less the act of refusal, of physicians who object to participating in EAS.
(*EDITED An earlier version stated that licences were at risk. Not yet.
BBN 11 February 2020 12:30 AM)
More thoughts on Texas Advance Directive Act
I was asked about the #BabyTinslee case and what we should do, what can we do, in the disputed cases.
We need to educate more. People don’t understand basic medical ethics in this day of “choice.”
Autonomy doesn’t supersede nonmaleficience. In other words, the First Principle of medicine, “Cure when possible, but first do no harm,” always should guide us, rather than “wants” or “choice.”
In the end, doctors are the ones actually performing the acts and we’re most likely to understand the projected outcome. We benefit from oversight by colleagues and the community, both informally and in the process prescribed by the Texas Advance Directives Act.
Some people demand that every one of these cases go to court, for “due process” and “cross examination.”
But judges and courts can’t be as knowledgeable as doctors are. Their decisions are necessarily informed by dueling (paid) lawyers and (hired) medical experts.
In all the cases that have gone to court, the family has had quite a lot of notice, but the 48 hour notice before the committee meeting is perceived as too abrupt, especially since the relationships all appear to be adversarial by that point.
(And who could get your family to a meeting in 2 days?)
The 10 days isn’t thought to be long enough to arrange a transfer, either. Again, in many of the Court cases, the attempts to find another doctor willing to accept the patient’s care has begun before the committee meeting.
Doctors acknowledge the great trust and privileges we are given by agreeing not to abandon our patients. When we have a disagreement with a patient or surrogates (usually a familymember), we accept that we must continue treatment for a period of time. But not indefinitely.
If we could get the reforms that have been attempted to lengthen the statutory timeframe (multiple times) since before 2005, the TADA would be much better. It’s still the best process we have, currently.
Miracles in a predictable universe
We are blessed with a universe that’s predictable and testable, yet we pray for miracles. And we pray for miracles, but act as though human actions can block them. Is the will of the Creator Who spoke the physical laws into existence limited by humans if they act as though the universe is predictable and testable?
Those of us who practice medicine are limited by the physical laws, the predictable and testable, with an emphasis on the tested. Our education and experience is based on these tested predictions and guide our decisions, and we’re watched and sometimes redirected by our colleagues, patients, laws and the community.
And then, there’s the best test of all: time.
In fact, I once noted that a patient who outlived the “10 Day Rule” might have proved the doctor (who instigated the process from the Texas Advanced Directive Act) wrong. There might have been a few cases like this, just as I believe there have been miracles.
However, can you tell me how to measure these events and predict their occurrences, much less practice medicine based on them?
In the majority of TADA cases when treatments weren’t withdrawn, the patient died in the exact manner the doctors predicted, after the same interventions -and sometimes more invasive and tortuous “treatments” than the ones the doctor originally objected to.
Doing to, not for (Baby Tinslee & TADA)
“We’re doing things to her. Not for her.” (Wini King, spokesperson for Cook’s Children’s Hospital, January 3, 2020) This may be the best description of a very sad case.
Tinslee Lewis was born prematurely on February 1, 2019, with severe heart and lung defects. She had cardiogenic shock and was admitted to the Cardiac ICU at Cook’s Children’s Hospital immediately. ♡(See Cardiac Pathology ♡below.)
Even after three open heart surgeries, a fourth to close her sternum, a short time on ECMO (essentially, heart-lung bypass) and constant ventilator since July, of 2019, Tinslee’s enlarged heart and small, damaged lungs can’t keep up with the necessary blood circulation and exchange of oxygen and carbon dioxide, even with the assistance of multiple blood pressure medicines, diuretics and the ventilator on high, except when she’s still and quiet with the help of sedating and paralyzing drugs.
In response to a lawsuit against Cook’s Children’s Hospital, where Tinslee has been in the CICU since birth, Tinslee’s medical records were submitted to the Court. I’ve been able to review approximately 200 pages that are now public record, describing the constant, repetitive interventions necessary to keep Tinslee alive on the ventilator.
Tinslee’s doctors (and, the notes show, the nurses and staff) believe that they are being forced to cause Tinslee pain and suffering, while keeping her paralyzed and sedated. They report increasing difficulty with managing the ventilator so that her damaged heart & lungs can maintain oxygenation. She requires repetitive heart, lung and blood tests to guide adjustment of meds & treatments and has had several infections requiring treatment. In contrast to my earlier presumption, the notes in the records show that the ventilator and all its required meds and manipulations are indeed causing undesired problems, including fluid overload, infections and cardiopulmonary distress, in addition to her underlying lung disease. Even the baby’s growth, something we usually celebrate, increases her risk of cardiopulmonary insufficiency.
Those records also contain notes from many attempts to explain and council Trinity Lewis, Tinslee’s mother, about her baby’s underlying problems and prognosis and the reasoning behind, in contrast to some past media reports.
Ignoring the fact that doctors, not hospitals, practice medicine in Texas, Texas Right to Life Lawyer Joe Nixon is quoted, claiming that the “hospital ” has decided to withdraw treatment. Texas Attorney General, Ken Paxton, is shown to have Tweeted that the problem is a “legal issue,” rather than an ethics and justice matter of forcing doctors (and by their orders, nurses and other staff) to cause pain and suffering for a little girl who is dying as her body fails to heal, in spite of every intervention possible.
Many people, out of compassion, object that “the family ” should decide when to withdraw life support. Yet, the family members aren’t watching the oxygen levels drop while they rinse Tinslee’s airways with a bicarbonate solution to keep her lungs clear. And it’s certainly not the lawyers that are probing, injecting, measuring and adjusting constant, innumerable hourly interventions done to a baby who must be sedated and paralyzed to prevent cardiac and respiratory distress.
In spite of the diligent complicated interventions and care of the doctors and nurses at Cook’s, there have been comments in blogs and social media that the “hospital” wants to “kill” Tinslee. Startlingly, AG Paxton called the latest Court ordered, indefinite hold on removal of life support a “Stay,” as though the doctors, not her multiple medical problems, would kill Tinslee. He also misrepresents the process that Cook’s Children’s Hospital and Tinslee’s doctors followed,
“The statute fails to require that physicians provide an explanation of why they refused life-sustaining treatment and provide the patient’s family with adequate notice and opportunity to argue their position prior to the committee reaching a decision, effectively allowing the government to deny an individual’s right to his or her own life and to do so without due process.”
In fact, though, it is the lawyers, particularly at Texas Right to Life, who are turning a little girl’s tragedy into a continuation of their legal battle against the Texas Advance Directive Act. I’ve covered the benefits of and the struggle to improve the Act – repeatedly blocked by TRTL and their lawyers – for years on both WingRight.org and Lifeethics.org
The Act, TADA, was hammered out in 1999 by a group of stakeholders including patient and disability advocates, hospitals, doctors, ethicists and lawyers. Texas’ prolife organizations, including TRTL and the organization for which I served on the Board of Directors for 15 years, Texas Alliance for Life, and for whom I wrote this essay.
Briefly, TADA allows a balance and legal options when there’s a difference in opinion between a patient’s desire for a given treatment and the medical judgment (a combination of education, experience, and the standard of care) of the doctors who are tasked with the most difficult medical and surgical cases.
I’ll admit that it’s my opinion – and only my opinion – that the lawyers hate that TADA provides a safe haven from lawsuits if doctors follow the law (!). I slowly came to this conclusion over the years because at virtually every Legislative hearing and stakeholders’ meeting about any changes to the Act, the lawyers bemoan the fact that doctors don’t have to go to court over each of these cases and that they face no legal penalty or “liability.”
Poor Tinslee Lewis will most likely never leave the hospital alive. Disease and death don’t respect “due process,” but, they are predictable and an inevitable part of life. Hopefully, we will see her mother and those who love her come to find peace with her death, celebrating the time they’ve had to be with her, especially these last 2 months. However, I fear that the lawsuits will continue for years, adding to their grief.
Edited 1/19/2020 for a typographical error: in the secondparagraph, “cardiogenic” replaced “carcinogenic.” BBN
♡Ebstein Anomaly – Cardiac Pathology 101, about as simple as I can make it (and understand, too);
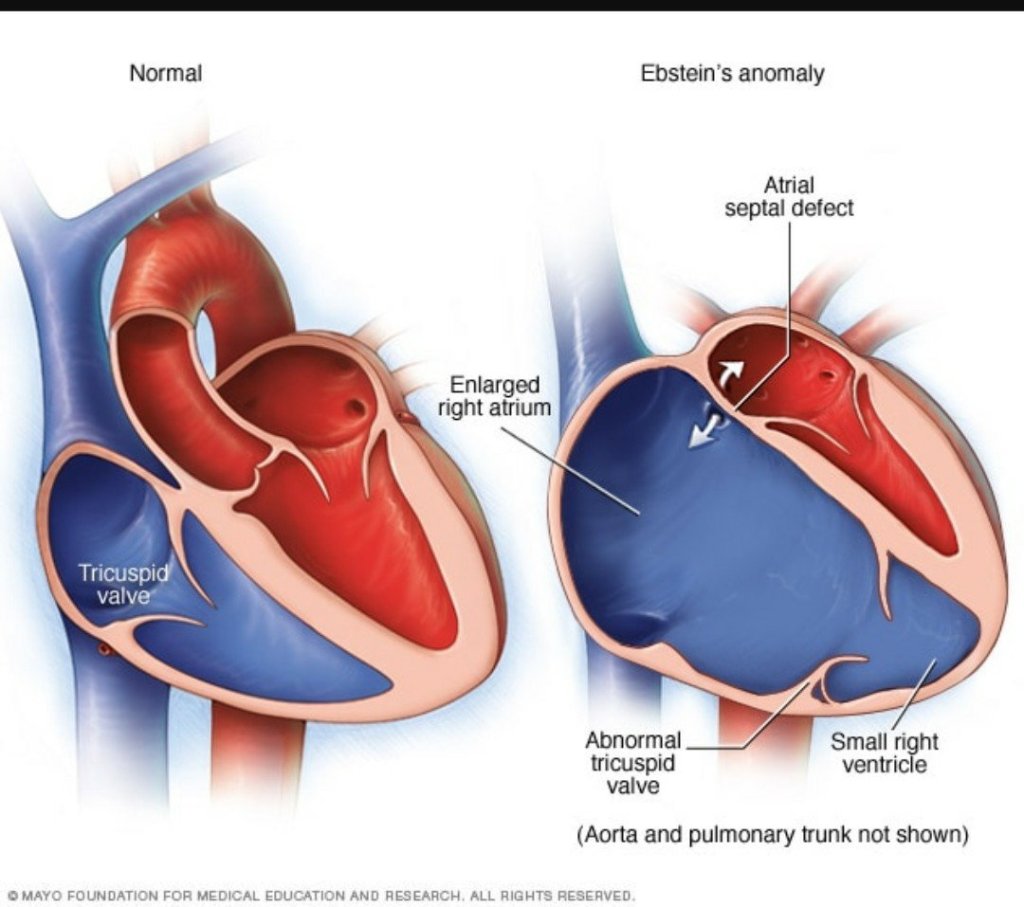
(Thanks to Mayo Clinic)
Babies born with Ebstein Anomaly have a malformed right and atrium and ventricle and misplaced (tricuspid) valves between the right sided ventricle and atrium. The larger right ventricle can’t pump efficiently.
In addition, the blood the right ventricle tries to pump into the lungs leaks/flows/churns (risking blood clots) back into the right atrium, which grows even bigger, with even thicker walls. The ventricle also grows bigger. When the muscle fibers of the chamber walls get stretched apart enough, they are less inefficient. (Think of two hands gripping at the fingers. The farther out the grip, palm > 1st joint > fingertips, the less strength and pull on the opposite hand.) (For the geeks: Frank-Starling law.
The lungs aren’t efficiently filled with blood, they don’t expand, the pressure builds up in them and efficient exchange of gasses doesn’t take place.
In the meantime, the blood backs up in the body, the liver, kidneys and extremities & eventually the left side of the heart, which can hypertrophy , too.
The enlarged heart puts pressure on the lungs and nearby soft tissue, including the blood vessels coming to the heart.
The combination of leaking high pressure blood vessels and the body’s increasing fluid in order to try to pump what oxygen there is, leads to edema or swelling of the body.
Sometimes, the fetal atrial-septal defect stays open, allowing mixing of the un-oxygenated blood from the right, with the oxygenated blood. This malfunction can help, temporarily.
With the high pressure, poor flow, and actual physical damage due to the mass of the heart, none of the organs can function well. Increased activity, stress, and growth will increase the demand for oxygen, kidney & lung function.
Cook’s Children’s Press Release on Tinslee Lewis
The Press Release is published in .pdf on the hospital’s website. Here’s the text:
Cook Children’s Statement Regarding Patient Tinslee Lewis Fort Worth, Texas (November 10, 2019) –
Tinslee Lewis is a beautiful baby who has captured the hearts of many at Cook Children’s since her premature birth nine months ago. She was born with a rare heart defect called an Ebstein’s anomaly and has undergone several complex surgeries at Cook Children’s in an effort to improve her heart function. Further complicating matters, she also suffers from chronic lung disease and severe chronic pulmonary hypertension. Due to these complications, she has spent her entire life hospitalized in Cook Children’s intensive care unit. She has required artificial respiratory support throughout that time, and has been consistently on a ventilator since July.
In the last several months, it’s become apparent her health will never improve. Despite our best efforts, her condition is irreversible, meaning it will never be cured or eliminated. Without life-sustaining treatment, her condition is fatal. But more importantly, her physicians believe she is suffering.
To maintain the delicate balance necessary to sustain Tinslee’s life, and to prevent her from pulling out the lines that are connected to the ventilator, doctors have had to keep her constantly paralyzed and sedated. While Tinslee may sometimes appear alert and moving, her movements are the result of being weaned off of the paralyzing drugs. We believe Tinslee is reacting in pain when she’s not sedated and paralyzed.
Cook Children’s has made heroic efforts to treat Tinslee’s condition, all while being very transparent with her family regarding her poor prognosis. Despite those extraordinary efforts, Tinslee’s condition has not improved. At the request of Tinslee’s family, we have reached out to nearly 20 facilities across the country to see if any would be willing to accept Tinslee as a patient. Some of the facilities include:
Texas Children’s Children’s Memorial Hermann Hospital Dell Children’s Dallas Children’s Medical City Dallas Children’s Medical Center Oklahoma City Children’s Hospital of Atlanta St. Louis Children’s Children’s Hospital of Philadelphia Johns Hopkins Methodist Hospital San Antonio University Hospital San Antonio Boston Children’s Children’s Hospital of Los Angeles Arkansas Children’s C.S. Mott Children’s Michigan LeBonheur Children’s Memphis Rady Children’s Children’s Hospital San Antonio CHRISTUS
All have said our assessment is correct and they feel there is nothing more they can provide to help improve this precious child’s life.
A team of Cook Children’s doctors nurses and staff have given their all to help Tinslee. While, we believe every child’s life is sacred, we also believe that no child should be sentenced to a life of pain. Removing this beautiful child from mechanical ventilation is a gutwrenching decision for Cook Children’s physicians and staff, however we feel it is in her best interest to free her from artificial, medical intervention and suffering.
Winifred King
Assistant Vice President of Public Relations Cook Children’s Health Care System
Baby Tinslee Lewis and the Texas Advance Directive Act
I was a relieved to hear that the doctors caring for 9 month old Tinslee Lewis decided not to remove her ventilator on Sunday, November 10, 2019. Their decision, most likely due to public outcry, was announced 2 hours before removal was planned. Later in the day, and a local judge issued a restraining order that mandates continuing the ventilator until at least November 22 unless an appropriate transfer to another facility can be arranged.
At first glance, this sounds like several other stories about disputes between the family of a patient and medical professionals who have invoked the provision in the Texas Advance Directives Act(TADA) that allows for removal of life sustaining treatment. However, from what I’ve read and the hospital’s statement, I’m concerned that this time the law may have been invoked based on “quality of life” rather than the futility of the treatment and the suffering it causes.
(Note: I want to be very careful to point out my limits. The following medical and legal information about this case comes from what I’ve gleaned from Facebook, blogs and Twitter posts, as well as a few news articles like this one. I’ve tried to be as factual and accurate as possible. It’s important to understand that I don’t know all the details and that any conclusions I draw are merely my opinion.)
Tinslee has lived her whole life in the ICU at Fort Worth Cook’s Children’s Hospital. She was premature and was diagnosed with a congenital heart defect, Epstein’s anomaly, that in spite of several surgeries led to heart failure and caused her heart to become so enlarged that it damaged her lungs. She’s been on a ventilator since July.
Her doctor or doctors reportedly believe that Tinslee is in pain and suffering. In order to keep her comfortable and to prevent her pulling the ventilator and feeding tubes, they must use paralyzing drugs and sedation. An attending doctor responsible for Tinslee’s care invoked TADA and a hospital committee agreed that the continued use of the ventilator is inappropriate. On October 31, the family was notified that the ventilator would be discontinued at 5 PM on November 10.
I became concerned when I saw the video posted at Texas Right to Life, showing a beautiful girl with apparently healthy skin, reacting to voice and touch. In the video, she doesn’t move her right leg, barely opens eyes and only seems to point her eyes to lower right. Still, the treatments, including sedation, seem to be working and she doesn’t appear to be in distress or pain.
A hospital spokesperson, Winifred King, assistant vice president of public relations for Cook Children’s Health Care System, sent out a statement by email, that is quoted in part by the Fort Worth Star Telegram:
“In the last several months, it’s become apparent her health will never improve,” King said in a statement via email. “Despite our best efforts, her condition is irreversible, meaning it will never be cured or eliminated. Without life-sustaining treatment, her condition is fatal. But more importantly, her physicians believe she is suffering.”
And,
“While we believe every child’s life is sacred, we also believe that no child should be sentenced to a life of pain,” said Winifred King, assistant vice president of public relations for Cook Children’s Health Care System, in a statement. “Removing this beautiful child from mechanical ventilation is a gut-wrenching decision for Cook Children’s physicians and staff; however, we feel it is in her best interest to free her from artificial, medical intervention and suffering.”
(Kaley Johnson, Fort Worth Star Telegram https://www.star-telegram.com/news/local/fort-worth/article237223826.html accessed 11/10/19)
Hesitantly, I find myself second guessing the decision of Tinslee’s doctor(s) to invoke TADA and of the hospital ethics committee to affirm that the ventilator is inappropriate medical care. As I wrote above, I can’t know the real medical circumstances and certainly haven’t examined Tinslee or even read her chart. I’m not a pediatric cardiologist or pulmonologist and may not understand her prognosis as she grows and develops. Has she required chest tubes because of the ventilator? Is she growing? Will a larger body put too much strain on her heart or will growth allow time – and room – for her lungs to heal? Will she be able to have a tracheostomy and would it make her care easier and her more comfortable?
However, there’s no sign that the ventilator itself is causing damage to her lungs and there is evidence that the medication helps Tinslee tolerate the mechanical intervention.
The wording of Ms. King’s statement makes it appear that the doctor(s) decided to end the ventilator treatment based on a perception of her quality of life, rather than on their knowledge of the futility of the treatment and the damage it causes. In my opinion, “quality of life” is a very personal value judgement. As I’ve noted before,
“Although no reason is required by law, in every case I know of the doctor has made it clear that the requested treatment is causing suffering and/or actual harm and violates the First Principle: “Cure when possible, but first, do no harm.”’
The good news is that TADA allows, and Tinslee’s family were able to, access practical and legal assistance.
Ms. King shared a list of 19 hospitals that, as required by TADA, the hospital administration has contacted in an attempt to find other doctors and facilities that will accept Tinslee as a patient. All refused the transfer, apparently agreeing with Tinslee’s doctor (and casting doubt on my conclusion).
TADA also allows the family to seek a delay through the local courts. Texas Right to Life helped Tinslee’s family by providing a lawyer and legal advice. They also sent out a plea on Friday, November 8, asking the public to call and email Cook’s administrators about Tinslee. Several State legislators have also become involved.
Now, Tinslee’s mother and family and the hospital will have another 12 days to try to find someone willing and able to treat her.
Questions still remain: Is there any long term facility that is able to offer the ventilator and sedation that Tinslee needs? Or must Tinslee live sedated and paralyzed in the ICU for the rest of her life?
But there shouldn’t be any question weighing whether Tinslee’s “quality of life” is worth living.
Updated information on TRTL, end of life, and money
One Texas Right to Life (TRTL) lawyer has posted an update on Facebook about the “rescue” of Mrs Carolyn Jones. I’m afraid that, as with the declaration that another patient was “slain,” TRTL is gaming the Medicare funding and Texas medical systems for political purposes.
Emily Cook, General Council for TRTL, wrote that she worried that “funny business clinically would happen as we moved her” from the hospital where Mrs. Jones has been admitted for over 6 months, where the docs had weaned her off the ventilator and wanted her to transfer to a more appropriate level of care facility over 2 months ago.
Emily says TRTL spent their own money (*see my last paragraph) to put her in a private ambulance and take Mrs. Jones to another hospital ER. That hospital couldn’t provide dialysis, so they in turn transferred her via ambulance somewhere else, to yet another hospital until admission can be arranged at the nursing home.
Cook-ing the system
Mrs. Jones’ Medicare funding for the original hospitalization is bound to have run out some time ago. Normally, Medicare will allow 90 days per admission, with an extra 60 “reserve” days, once per person, per lifetime. The patient is responsible for part of the bill from the first day of admission, and for the total hospital costs after the eligible days.
But there are still Medicare regulations to deal with in the case of “Medicare eligible” patients, even when they aren’t paying.
Medicare makes it very difficult and risky for everyone to navigate the private pay process. When I had a question in my private medical office about whether Medicare would cover something, we had the patient sign an informed consent agreement and an acknowledgement that the patient might have to eventually pay if Medicare denied the service. Then we performed the service, filed the charge with Medicare, waited to be denied, and then tried to Bill the patient. I gave away a lot tetanus vaccines and removed a lot of moles and warts for free to avoid the risk of “fraud and abuse” from the likes of Janet Reno.
The same risk would have applied if the hospital had privately charged Mrs. Jones’ Dialysis.
I don’t believe the first new hospital is at risk for a charge of “dumping” if they documented a legitimate reason. However, both new hospitals will be able to charge the Jones copays and co-insurance. They may also find Medicare coverage limited because of the way Mrs. Jones left the original.
“Medicaid limits 2019” (a .PDF)
I certainly don’t know the Jones’ financial circumstances, and I may have over estimated the maximum income in early speculation. However, there are strict maximum Medicaid income and asset levels. These vary according to age, disability, and marital status. (Even the government bureaucratic Leviathan doesn’t want the spouse if a nursing home patient to end up indigent.)
In my experience, the social workers and benefits experts at hospitals and nursing homes are experts at negotiating and translating the bureaucracy. In addition, the disabled Medicare eligible person will have access to a benefits specialist. I’ve never had a hospital discharge and nursing home admission blocked by this “paperwork.” Certainly not for months at a time.
I hope TRTL assists the Jones family with what is certain to be several enormous hospital bills. As long as they pay the bills directly, the funds won’t be counted as income to Mrs. Jones.
False story about Texas Advance Directives Act (TADA)
Mrs. Jones is not dependent on the ventilator.
In fact, it sounds like Mrs. Jones has had excellent treatment at the hospital,
Mr. Jones told the Texas Senate Health and Human Services Committee that the doctors at the hospital successfully weaned Mrs. Jones from the ventilator.
He also said that three other facilities are ready for her admission.
I’m happy to see that today’s article by reporter Tony Guajardo quotes both opponents and supporters of TADA and corrected the impression that Mrs Jones is dependent on the ventilator: “She requires dialysis, occasionally needs a ventilator for breathing assistance, and uses a feeding tube.“
And yet, today’s The Texan article still misrepresents this case: “UPDATE: Recovering Beaumont Woman’s Life-Sustaining Treatment to End Due to 10-Day Rule.”
There’s also a quote from Mrs. Jones’ daughter, repeated from the earlier article: ““My mom is going to die on Monday because of a law that saves hospitals money.”
It turns out that money and Medicaid paperwork is actually what is keeping the family from allowing Mrs. Jones to be transferred to another doctor and facility. The family is concerned that they (rather than the hospital) will be responsible for the costs of Mrs. Jones’ care.
This is in spite of the fact that when a patient first goes on dialysis, she becomes immediately and automatically eligible to apply for Medicare and Social Security Disability.
Depending on assets and income, patients unable to work on dialysis also qualify for Medicaid and other State benefits in Texas. Medicaid will even pay bills retroactively for three months.
The good news is that she isn’t dependent on the ventilator, dialysis is not constant but only 2-3 times per week and paid by Medicare, food and water by the feeding tube can’t be withheld under TADA.
Hopefully, the Jones family will finally agree to transfer her, even if costs them more than her Medicare & Social Security Disability will pay.
Have they no decency?
Now, Texas Right to Life is blatantly lying, posting an article on their website entitled “American hero slain two days before Christmas …”
“slain?”
Far down in the piece, there’s this:
“Chris passed away naturally on December 23, 2015 – two days before Christmas.”
Mr. Dunn died from his metastatic pancreas cancer, on full medical treatments. His mother, Mrs. Kelly actually thanked those who cared for him at the hospital.
Every article on TRTL’s website has a “Donate” button at the top, prioritizing money over the people whose stories they use to raise money and influence the Texas Legislature. Now, we see this completely dishonest caption.
Just what is their mission and how can we trust them?
Hurting patients and families
I don’t understand why TRTL repeats that a ventilator tube prevents Mrs. Jones from speaking or eating. Mrs. Jones has a tracheostomy in place (the tube we see in the pictures is a feeding tube). The tracheostomy, even when a ventilator is attached, would not interfere with her ability to speak and swallow, with training.
Emergency: Liberty Right Infringement
Texas Right to Life General Counsel Emily Cook is attacking Texas Medical Association on Facebook, even though virtually every other pro-life, medical, nursing, hospital, and disability group in Texas oppose SB 2089 by Hughes, that would change the “Texas Advance Directive Act, “TADA” will harm patients and attack the right of doctors to refuse to act against our conscience.
We’ve worked to fix other problems: Artificially administered food and water, even full IV feedings, can‘t be removed. Texas law didn’t even mention DNRs, but last session, we passed an amendment with explicit procedures and informed consent language.
There’s no leeway, at all, in the new Bill.
SB 2089 specifically says anyone can file a lawsuit in any Court in the County, the Court can’t charge the patient (or surrogates) any fees, and the judge is required to rule in 5 days.
If you believe that even doctors have the right of Conscience, and that infringement of the right not to be forced to act against your will is wrong, please contact your Texas Senator and Lieutenant Governor Dan Patrick and respectfully ask that SB2089 not be brought up.
You can let me know if you disagree on my Facebook page.
Another kind of lawyer joke
“[T]he doctor/bioethics committee thinks the patient should die.” Wesley J. Smith, Esq., Texas Senate Health and Human Services Committee, 4/10/2019 LifeNews.com
Wesley Smith is a rarity among the many lawyers who chased bioethics to the bedside late in the last century: he actually believes in the sanctity of human life and in the right of conscience. I’ve attended and reported on his debates and encounters with proponents of intentional euthanasia. And even happily defended him.
Unfortunately, Lawyer Smith was not above spinning the truth this month when he came from California to once again misrepresent the Texas Advance Directive Act (“TADA,” “the Act,” or “166.___”), an attempt to balance conflicting rights when doctors disagree with a patient or his surrogates about actual medical procedures and treatments that the doctor believes harms the patient.
On April 10, 2019 Mr. Smith gave invited testimony to the Senate Health and Human Services Committee in favor of SB 2089 (Hughes) and
SB 2129 (Creighton). LifeNews.com published part of his testimony online, under the title, “Texas Rule Allows Hospitals to Essentially Euthananize Patients After a 10-Day Notification.”
Mr. Smith doesn’t just contradict multiple Supreme Court rulings since Cruzan (1990) affirming that withholding or withdrawing treatment is not equivalent to euthanasia. Paradoxically, he echoes arguments that anti-conscience activists use to justify abortion on demand, Physician Assisted Suicide and intentional euthanasia by a third party by claiming that the principle of autonomy supercedes “First, do no harm,” or non-malevelence, and the right to conscience.
(You can watch all of Part I and Part II of the April 10, 2019 Health and Human Services Committee meeting addressing SB 2089 by Senator Bryan Hughes and SB 2129 by Senator Brandon Creighton online. Part I includes Mr. Smith’s testimony beginning at 33:00/1:01:10.)
We’ll skip Mr. Smith’s assertion that there is a right to force others to provide everyone medical care in general, not just in emergencies or at the end of life. I’ve covered these assertions and his attacks on the Texas Conference of Catholic Bishops I’m, back in 2007.
Today, let’s just look at his spin on the current version of TADA.
Lawyer Smith uses emotionally weighted terms that aren’t in TADA, such as, “life-extending,” “futile care,” “permitting the institution to force its will on patients and families,” “invidious discrimination,” and “inappropriate care.” He contrasts patient’s “rights” with doctor’s “values,” and is the first that day to raise the specter of doctors willing to kill when patients are “expensive.” And, reflected in the LifeNews.com headline, Mr. Smith flatly says that TADA allows euthanasia – intentional acts to kill patients – equivalent to the administration of injections or medications that he wrote about this week.
As I’ve stated so many times in past WingRight.org and LifeEthics.org posts, TADA doesn’t allow us to remove or withhold care for patients, only treatments that are “medically inappropriate.” There are no futile patients, only futile treatments that cause harm to the patient over and over, without any expectation of reversing organ failure after organ failure.
Mr. Smith also ignores the multiple attempts by the medical and pro-life community and Legislature to improve the law’s timeframe and communication, much as Senator Creighton’s Bill. One example from 2007, SB 439 by Senator Bob Deuell, would have required written notice and an offer of a private ethics consult to take place at least seven days before the hospital committee meeting. That Bill had a schedule for giving the patient or surrogates written information about the dispute process, copies of medical records, and lists of resources. The family would have been given access to the committee meeting, with their own advocates. When the committee agreed that the treatment requested was inappropriate, the family would have receive assistance in searching for7⅞ another doctor or facility for at least another 21 days. I believe that the Bill bogged down in the House because of opposition from Texas Right to Life to any Bill that did not include liability for doctors and the indefinite “treatment until transfer” in this year’s SB 2089.
In the last five minutes of the Part I video, another lawyer, Texas Right to Life General Council Emily Cook, gave us the best clue about the ultimate goal of her organization: “judicial review.”
Ms. Cook and Mr. Smith would have every one of these disputes settled by a Court. This is the Texas trial lawyers’ dream: a huge weapon against our State’s tort reform.
Today, the law specifically allows an appeal to a County probate judge when the Committee agrees with the doctor’s decision. SB 2129 allows a request for an injunction in any Court in the County, enabling “judge shopping.” Since it also prohibits the County from charging the patient or his surrogates any fees, the costs would fall solely on the County.
Ultimately, SB 2129 would make it much, much easier to sue the doctor and the hospital, moving Medical decision-making into the courtroom.
Most of the “stakeholders” for patient rights in Texas (including Texas Alliance for Life, Texas Baptist Christian Life Commission, Coalition of Texans With Disabilities, Texas Medical Association, Texas Hospital Association, Catholic Hospital Association, Texas Nurses Association, and the Texas Conference of Catholic Bishops and many others) oppose both of the Bills that Mr. Smith favored. Since SB 2129 would mandate that the County pick up any Court costs and that the judge make his ruling within five days, don’t be surprised if we hear objections from representatives of these parties, too.
So what’s the “joke?”
It could be the ridiculous notion that Lawyer Smith is a mind reader, able to discern the “invidious” motives for the “discrimination” he feels doctors and hospitals routinely practice:
“To fully comprehend the unjust nature of Texas law in this regard, realize that these “futile care” or “inappropriate care” decisions do not terminate treatment because it won’t work, but because it does. It is keeping the patient alive when the doctor/bioethics committee thinks the patient should die.” (Emphasis from LifeNews.com’s transcript.)
He repeatedly comments that physician’s decisions about medically appropriate treatment are subjective and that they (we) might “project their fears and their desires onto the patient” based on our “values,” rather than medical judgement based on repeated, at least once a day examination of the patient, reports by the nurses and staff and our education and experience.
The joke might be that Lawyer Smith volunteered that the indefinite, repeated evaluation and medical decision-making against the medical judgement of doctors would not be “slavery.” I would like to know what Lawyer Smith calls the legal requirement to use one’s body and brain to carry out actions, including writing orders for nurses and other medical staff, against your will.
It might be tragically funny to watch “judicial review” end up with the two sides hiring expert witnesses – doctors – to give the judge opposing views. There’s dark humor in the realization that ultimately the judge would order the original doctor to use her medical judgement to provide treatment – against her best medical judgement.
But the real joke is that “judicial review” risks the unintended consequence of decisions made by judges like the late t Judge George Greer, who Mr. Smith wrote about in this article.
Comments are closed. Please comment on my Facebook page.
Texas Advance Directive Act 2019 Legislature
“(22) in complying with the procedures outlined in Sections 166.045iand 166.046, Health and Safety Code, fails to make a reasonable effort to transfer a patient to a physician who is willing to comply with a directive.Amendment No. 5Representative Toth offered the following amendment to Amendment No. 4:Amend Amendment No.4 by Toth to CSHB 1504 on page 3, line 25, between “Code,” and “fails”, insert “willfully”.””
Banned by prolife website

I’ve sat on this for 4 days, hoping for a response to the questions I sent to 2 of the ‘co-founders” and an editor of the website. (They only use those online forms, so I can’t follow up by email.)
So far, no response from any of the 3.
I’m not going to link to the website, but the address is in the photo.
Unfortunately, the division in the Texas prolife community is deep. The article I attempted to comment on quotes – and disputes – an article I wrote for Texas Alliance for Life a few years ago.
All I wanted to say was that I hope the readers will read that article.
Praying for peace.
(BTW, that case ruling came down in favor of Houston’s Methodist Hospital and the Texas First Court of Appeals refused to declare the Texas Advance Directive Act unconstitutional.)
Response to criticism about Texas Advance Directive Act
I’ve been having a long Facebook discussion with representatives of organizations, people who claim that I support coercion and killing patients because I defend the Texas Advance Directives Act, 166.0046. (TADA).
I want to respond as fully as I can. ( I’m bandwidth deprived today and will gradually add more links when I reach better signals. See here, here, and here for more explanations from earlier WingRight posts. Links to the law, the press, and previous blog posts by others can be found in those articles.)
It was easy to follow this case. There was a video published by Texas Right to Life (TRTL), a lot of press, statements to reporters by family, lawyers, and TRTL staffers, as well as a couple of lawsuits. I spent the better part of two days once again reviewing the public records.
It
(Edited 03/11/18 for typos, to add a link, and to clarify points originally made on Facebook in a long debate. BBN)
Law makers to doctors: “Keep the patient alive”
If only we doctors – or legislators, lawyers and probate judges – really had the power to “keep the patient alive” as this article claims two new Bills ( HB 4090 & SB 1213) in front of the Texas Legislature will (force doctors to) do.
The article is misleading in its claim that a committee or a hospital decides whether or not a therapy is given: Texas doctors practice medicine in Texas. Even the Bills make it clear that the “attending physician” makes the decision whether or not to follow the patient’s (or more likely, the surrogates’) medical request.
We – Texas doctors, hospitals, and legislators – have tried repeatedly over the last decade to amend the law, Texas’ Advance Directive Act, to increase the time frame. Last Session, we helped to ensure that food and water can’t be withheld. The lawyers and those who would have Estate (probate) judges involved in every dispute – even at the bedside of the dying – have blocked effort after effort because the Bills did not include liability for the doctor.
These Bills are just the camel’s nose under the tent of Texas’s tort reform. Worse yet, we’d end up with medical expert testifying against medical expert in court, with the judge eventually telling the doctor how to practice medicine. It would also severe the “ethicists” who actively seek to undermine conscience protections for health care professionals.
If you’ll notice, the Bills also remove the requirement for the patient to pay for any transfer, too. I don’t suppose that the tort lawyers will pay for the ambulance or plane ride.
Do you want Texas law to force doctors to practice against our consciences?
How long and how far should any man or woman be forced by law to act against his or her will?
Would you like to refuse?
Shocking Bill from Texas’ Jason Villaba, Republican State Representative from Dallas’ District 114 : HB 1938 would make organ donation after death “opt out” for anyone applying for a driver’s license in Texas.
Texas would be the first State to pass such a law.
Organ donation is a public good for those who wish to do so. However, there is no ethical or legal precedent for treating human bodies – living or dead – as public property or commodities.
From the Bill as introduced:
(2) for an applicant who is 18 years of age or older: (A) specifically ask each applicant the question, “Would you like to refuse to join the organ donor registry?” and state, “If you answer ‘no’ to the previous question or do not answer the previous question, you consent to join the organ donor registry by performing either of those actions.”; and (B) if the applicant does not affirmatively refuse to be included in the registry under Paragraph (A), provide the person’s name, date of birth, driver’s license number, most recent address, and other information needed for identification purposes at the time of donation to the nonprofit organization contracted to maintain the statewide donor registry under Section 692A.020, Health and Safety Code, for inclusion in the registry.
http://www.legis.state.tx.us/tlodocs/85R/billtext/html/HB01938I.htm
Death Politics
Someone named Rich DeOtte has written a Facebook piece attacking friends of mine. Rich mocks Dr. Joe Pojman as “a rocket scientist” and “knucklehead” (needless to say, that’s not popular in the Nuckols household) and takes a slap at Kyleen Wright, of Texans for Life Coalition and the Texas Medical Association.
Dr. Joe Pojman, Ph.D., is indeed a “rocket scientist,” who gave up his original career path of aerospace engineering to sacrifice as founder and Executive Director of Texas Alliance for Life, an organization I’m proud to support and serve as a Board member.
Joe wrote the op-ed that Rich attacks in direct response to the “misrepresentations” in another, political op-ed piece by Emily Kebedeaux Cook on the Texas Right to Life Website. Joe only wrote about issues, and did not engage in name calling or derision. The only reason Emily and TRTL are mentioned is because she’s the author of the political opinion piece about the “decline in the Texas Legislature’s efforts to protect human Life.”
As Joe points out, the very document to which Emily refers refutes her position: Texas was named one of three “Life List All-Stars” for 2016 by the Americans United for Life.
Joe laid out the case that our Texas Legislature’s pro-life laws are most definitely not at a standstill: we are ahead of the Nation. Joe’s position that Texas leaders gave us many successes in the 2015 84th Legislature is supported by the similar list of “Wins” reported by the Texas Catholic Conference, representing the Bishops of Texas. In an earlier letter, TCC notes that many of the criticisms Emily makes in her February 8th blog post were not previously scored “equitably” by TRTL. For instance, Senator Bob Deuell received no credit for authoring much of what became HB2.
In fact, Texas’ Legislative leadership in passing pro-life laws is why many of us are going to Washington, DC on March 2nd to bear witness when the Supreme Court hears testimony on the abortion facility regulations in HB2.
Emily and Rich focus most of their criticism on the efforts of pro-life groups, including doctors like me, to reform end of life care and the Texas Advance Directive Act (TADA). Session after session since it was passed, we in the pro-life community have had our efforts repeatedly blocked by the “death panel” accusations Rich makes and the demands in Emily’s op-ed.
I was one of the doctors appointed to the Texas Medical Association ad hoc committee that evaluated last sessions’ end of life Bills for TMA approval. Our group of doctors agreed to and helped fine tune HB 3074, what Emily called a “modest protection”: prohibiting the removal of Artificially Administered Nutrition and Hydration, including food and water by invasive medical methods like IV’s and “Total Parenteral Nutrition.” We were called anti-life and pro-“death panel” (Rich’s words) for including medical exceptions for the rare circumstances when the patient can’t process the AANH and/or when it actually caused harm.
Those “three strongest Pro-Life bills” that Emily mentioned were included in the “Wins” listed by the TCC. The Bills not only would have forced doctors to continue to indefinitely perform acts that we believe are not medically appropriate as long as a patient or his family demands it. They would have forced all disputes between the doctors practicing medicine and patients or their families into court and add “liability”(civil and criminal penalties) for the doctor.
Forget if you can, that if all disputes go to court judges would be required to determine medical care – to practice medicine – probably based on the testimony of dueling, paid medical expert doctors. Malpractice rates will go up for doctors taking on the most vulnerable patients – the elderly, the trauma victims and the victims of cancer. Those doctors will spend more time in courts, rather than in the ICU. And so will more grieving families.
We found out what happens when malpractice goes up in Texas, before tort reform was passed. Because of the malpractice crisis, there were no neurosurgeons west and south of San Antonio and Houston – none at all in El Paso or all of South Texas. We were losing obstetricians and family doctors willing to deliver babies and offer prenatal care, all over the State.
I don’t know how to translate past physician shortages directly into the possible shortage of doctors providing end of life care. However, I will predict that fewer family doctors, internists, pulmonologists and the ICU intensivists will be able to afford to practice in the ICU. Just as a patient had to be flown to Dallas, San Antonio or Houston from most of Texas for a head injury, only the tertiary medical centers in those cities will be able to staff their ICU’s properly.
Physicians, not hospitals – and certainly not courts – practice medicine in Texas. Doctors must be allowed to practice medicine according to our medical judgment, which is a combination of education and experience, under the watchful eye of the community; not “death panels,” but fellow physicians, nurses, ethicists, lawyers (who may be any of the former) and lay people. In the end, if you force the hands and minds of doctors against their judgment, you will end up with doctors practicing without judgment, and humans with inalienable rights forced to act against our will and in violation of our conscience.
And, now, back to Rich’s Facebook post. Think twice when you read political posts full of personal attacks and name calling. We should be able to discuss politics without, as Emily said in her blog post, “unnecessary, vicious, and vindictive fights inside the Republican Party.”
Edited to fix a name glitch – BBN
The Ethics of Texas’ Advance Directive Act
Laws relating to medical ethics debates are generally behind medical advances.
Unfortunately, those debates often become emotional and heated, and the individuals who are affected often face the “hard questions” of ethical dilemmas while reacting to life and death emergencies. When law-making is controversial, it’s best to go back to the basics of ethics for guidance: the inalienable rights to “Life, Liberty and the Pursuit of Happiness,” the Declaration of Independence, and Constitution.
All laws limit our rights, but good laws are based on the fact that these inalienable rights are negative rights: they are meant to prevent one person – or the government – from infringing the rights of another. Ethical laws strike a balance between seemingly conflicting rights. They prohibit or punish harmful actions, but they don’t compel a desired action against the will.
However, since there is a hierarchy of rights (the right to life trumps the right to liberty and property, liberty trumps property, etc.), there are very rare circumstances when it is appropriate for laws to compel individuals to act for the benefit of another. These laws should only go so far as to protect the life and freedom of the vulnerable patient or client, for a limited time with the goal of allowing safe transfer of the obligation to someone else.
For instance, parents are required to care for and protect their minor children since they are helpless and unable to legally consent or make contracts. And State laws require that doctors and lawyers be licensed, obtain certain levels of education, and follow specific, positive actions when they wish to withdraw from a professional relationship with or refuse the request of a patient or client.
That brings us to the controversy over the Texas Advance Directive Act of 1999 (“TADA” or “the Act”). In addition to describing “Advance Directives to Physicians” (also known as a “Living Will), TADA also attempts to outline the procedure for resolving any disagreement between a doctor and patients or their surrogates regarding medical treatments, especially concerning end of life care.
When I first read the Act, I (naively) thought it was malpractice protection for doctors who did not want to withdraw or withhold care. There have actually been a few “wrongful prolongation of life” lawsuits against doctors who – knowingly or not – used CPR when the patient had a Living Will.
Most of the time, however, TADA is invoked when the attending physician “refuses” a request to actively administer medical treatment that he or she believes is medically inappropriate. The steps laid out in the law involve the doctor’s notification of his refusal to the patient or the surrogate, the rules for assisting with transfer of care to another doctor who believes the treatment request is appropriate, and asking for a medical or ethics committee to be convened at the hospital. If no other willing doctor can be found and the committee agrees with the doctor, the treatment can be withheld or withdrawn (after 10 days). During that time, full life-sustaining treatment must continue and the hospital is required to provide medical records and to actively assist in looking for another doctor and/or hospital.
The law does never allow patients to be killed by intentionally stopping breathing. The law does prohibit withholding of pain medicine or comfort care and the removal of “artificially administered nutrition and hydration.”
Medical judgment is how doctors utilize our education, experience, and consciences as we plan and anticipate the effect of each medical intervention or treatment. “Life sustaining treatments are not “basic” or “usual care.” Nor are they one-time events without consequences. The interventions require a physician to administer and maintain. They must be monitored by observation and tests, and adjustments need to be made intermittently so that the treatment is effective and not harmful. They may lead to further more invasive and aggressive interventions and the need for the skills of other doctors in other specialties.
In some cases, patients and their advocates report trouble finding other doctors willing to provide the treatment that the first doctor thought was inappropriate. In my opinion, that difficulty is due to physicians’ common education and shared experiences – to medical reality, not ill intent.
Texas law is clear that only doctors may practice medicine by diagnosing and treating patients directly or “ordering” other medical personnel. Although TADA outlines specific duties for hospitals and hospital medical or ethics committees who determine whether or not the care is medically inappropriate, the process can only be invoked by the “attending physician” who is being asked to act against his medical judgment. The committee acts as a safeguard, to uphold medical ethics and the standard of medical care. In a formal meeting, the committee members review the case and either agree or disagree with the doctor as to whether he or she is correct about what is “medically inappropriate” treatment, for the patient.
Unfortunately, the Act has become known as the “Texas Futile Care Law,” and divides even the pro-life community. One side claims that doctors, hospitals and hospital committees are biased and should not be allowed to determine medically inappropriate care, and that doctors are obligated to give any and all desired treatment “until transfer.” Others want each case to go to court, where lawyers, judges and juries would settle every difference of opinion about “medically appropriate treatment.”
Ultimately, even the lawyers would need to consult doctors, unless the judges start writing orders for doctors, nurses, and medical professionals.
Our laws normally prohibit actions and only very rarely compel people to act. Under the conditions laid out in TADA, it is possible that the doctor can be forced to act against his medical judgment, but only for a limited, stated period of time. TADA is an attempt to balance conflicting rights: the patient’s wishes for medical intervention with liberty of the physician to practice medicine to the best of his judgment and conscience.
(Edited 03/11/18 to add a missing quotation mark. BBN)
Texas Advance Directive Act, when the doctor refuses
Here’s Section 166.046 of the Texas Advance Directive Act, the part of Texas Law that is in the news, these days. This part only applies when there is a disagreement between the doctor (whom the patient wants to continue treatment) and the patient or his surrogate about treatment decisions.
Sec. 166.046. PROCEDURE IF NOT EFFECTUATING A DIRECTIVE OR TREATMENT DECISION. (a) If an attending physician refuses to honor a patient’s advance directive or a health care or treatment decision made by or on behalf of a patient, the physician’s refusal shall be reviewed by an ethics or medical committee. The attending physician may not be a member of that committee. The patient shall be given life-sustaining treatment during the review.
(b) The patient or the person responsible for the health care decisions of the individual who has made the decision regarding the directive or treatment decision:
(1) may be given a written description of the ethics or medical committee review process and any other policies and procedures related to this section adopted by the health care facility;
(2) shall be informed of the committee review process not less than 48 hours before the meeting called to discuss the patient’s directive, unless the time period is waived by mutual agreement;
(3) at the time of being so informed, shall be provided:
(A) a copy of the appropriate statement set forth in Section 166.052; and
(B) a copy of the registry list of health care providers and referral groups that have volunteered their readiness to consider accepting transfer or to assist in locating a provider willing to accept transfer that is posted on the website maintained by the department under Section 166.053; and
(4) is entitled to:
(A) attend the meeting;
(B) receive a written explanation of the decision reached during the review process;
(C) receive a copy of the portion of the patient’s medical record related to the treatment received by the patient in the facility for the lesser of:
(i) the period of the patient’s current admission to the facility; or
(ii) the preceding 30 calendar days; and
(D) receive a copy of all of the patient’s reasonably available diagnostic results and reports related to the medical record provided under Paragraph (C).
(c) The written explanation required by Subsection (b)(4)(B) must be included in the patient’s medical record.
(d) If the attending physician, the patient, or the person responsible for the health care decisions of the individual does not agree with the decision reached during the review process under Subsection (b), the physician shall make a reasonable effort to transfer the patient to a physician who is willing to comply with the directive. If the patient is a patient in a health care facility, the facility’s personnel shall assist the physician in arranging the patient’s transfer to:
(1) another physician;
(2) an alternative care setting within that facility; or
(3) another facility.
(e) If the patient or the person responsible for the health care decisions of the patient is requesting life-sustaining treatment that the attending physician has decided and the ethics or medical committee has affirmed is medically inappropriate treatment, the patient shall be given available life-sustaining treatment pending transfer under Subsection (d). This subsection does not authorize withholding or withdrawing pain management medication, medical procedures necessary to provide comfort, or any other health care provided to alleviate a patient’s pain. The patient is responsible for any costs incurred in transferring the patient to another facility. The attending physician, any other physician responsible for the care of the patient, and the health care facility are not obligated to provide life-sustaining treatment after the 10th day after both the written decision and the patient’s medical record required under Subsection (b) are provided to the patient or the person responsible for the health care decisions of the patient unless ordered to do so under Subsection (g), except that artificially administered nutrition and hydration must be provided unless, based on reasonable medical judgment, providing artificially administered nutrition and hydration would:
(1) hasten the patient’s death;
(2) be medically contraindicated such that the provision of the treatment seriously exacerbates life-threatening medical problems not outweighed by the benefit of the provision of the treatment;
(3) result in substantial irremediable physical pain not outweighed by the benefit of the provision of the treatment;
(4) be medically ineffective in prolonging life; or
(5) be contrary to the patient’s or surrogate’s clearly documented desire not to receive artificially administered nutrition or hydration.
(e-1) If during a previous admission to a facility a patient’s attending physician and the review process under Subsection (b) have determined that life-sustaining treatment is inappropriate, and the patient is readmitted to the same facility within six months from the date of the decision reached during the review process conducted upon the previous admission, Subsections (b) through (e) need not be followed if the patient’s attending physician and a consulting physician who is a member of the ethics or medical committee of the facility document on the patient’s readmission that the patient’s condition either has not improved or has deteriorated since the review process was conducted.
(f) Life-sustaining treatment under this section may not be entered in the patient’s medical record as medically unnecessary treatment until the time period provided under Subsection (e) has expired.
(g) At the request of the patient or the person responsible for the health care decisions of the patient, the appropriate district or county court shall extend the time period provided under Subsection (e) only if the court finds, by a preponderance of the evidence, that there is a reasonable expectation that a physician or health care facility that will honor the patient’s directive will be found if the time extension is granted.
(h) This section may not be construed to impose an obligation on a facility or a home and community support services agency licensed under Chapter 142 or similar organization that is beyond the scope of the services or resources of the facility or agency. This section does not apply to hospice services provided by a home and community support services agency licensed under Chapter 142.
Added by Acts 1999, 76th Leg., ch. 450, Sec. 1.03, eff. Sept. 1, 1999. Amended by Acts 2003, 78th Leg., ch. 1228, Sec. 3, 4, eff. June 20, 2003.
Amended by:
Acts 2015, 84th Leg., R.S., Ch. 1 (S.B. 219), Sec. 3.0503, eff. April 2, 2015.
Acts 2015, 84th Leg., R.S., Ch. 435 (H.B. 3074), Sec. 5, eff. September 1, 2015.
Lawyers, politics, and end of life
- Two days before Christmas, 46 year old Chris Dunn died in the ICU at Houston’s Methodist Hospital. Almost everything you’ve read and heard is a deliberate, political skewing of the facts.
Texas Right to Life turned Mr. Dunn’s imminent death from metastatic pancreatic cancer into a crusade against the Texas Advance Directive Act (TADA or the Act). The Act is invoked by the attending doctor – not the hospital or ethics committee – when family members demand that he or she perform acts that go against the conscience because they are medically inappropriate, causing the patient to suffer without changing his course.
In this case, the mother and father disagreed with one another about the care plan and the patient was unable to make legally binding decisions. The father agreed with Mr. Dunn’s doctors that the treatment was causing suffering, objected to surgery to place a tracheostomy, and wanted hospice and comfort care. The mother wanted dangerous, painful procedures performed that would not change the medical outlook except to possibly hasten death.
And, unless you read the court records, you wouldn’t know that the judge ruled that Chris was not mentally competent to make his own medical decisions, that the hospital never wanted guardianship and had voluntarily promised to continue care until the guardianship could be settled. In fact all the lawyers, including the Texas Right to Life representatives, signed off on an agreement acknowledging this promise on December 4th.  ( The official court records are available to view free of charge online at the Harris County District Clerk’s website as protected pdf images. See Family case number 2015- 69681.)
( The official court records are available to view free of charge online at the Harris County District Clerk’s website as protected pdf images. See Family case number 2015- 69681.)
Inflammatory headlines falsely claimed that “the hospital” had imposed a “death sentence,” and was actively trying to kill Mr. Dunn by refusing to diagnose, treat or even give a prognosis. That same blog post mentioned non-standard treatments that some in the family were demanding.
First of all, of course there was a diagnosis. Several, in fact. From the signed affidavit of Mr. Dunn’s attending physician, filed December 2, 2015 in response to the law suit:
“Based on my education, training, experience, as well as my care of Mr. Dunn, I, and members of my team, have advised his family members that Mr. Dunn suffers from end stage liver disease, the presence of a pancreatic mass suspected to be malignant with metastasis to the liver and complications of gastric outlet obstruction secondary to his pancreatic mass. Further, he suffers from hepatic encephalopathy, acute renal failure, sepsis, acute respiratory failure, multi-organ failure, and gastrointestestinal bleed. I have advised members of Mr. Dunn’s family that it is my clinical opinion that Mr. Dunn’s present condition is irreversible and progressively terminal.”
The primary diagnosis was metastatic pancreatic cancer. The cancer was a mass that blocked the ducts and blood vessels coming from the liver as well as the normal function of the intestines. As liver excretions backed up into the liver and the blood pressure in the liver increased, Mr. Dunn suffered a life-threatening gastrointestinal bleed, fluid buildup in the abdomen and lungs, and sepsis (an overwhelming infection). All of these would aggravate respiratory failure, the necessity of a ventilator and lead to the kidney damage. Liver failure often results in hepatic encephalopathy and variable delirium.
There was definitely treatment given, including tube and IV feedings, antibiotics, the ventilator, and periodic removal of the abdominal fluid. Again, this was all publicly documented in Court documents, in the media and even on the Texas Right to Life blog that claimed that “Houston Methodist has invested no time or effort in Chris’s health, instead exerting their energies into trying to kill him instead.” [sic]
The Intensive Care doctors as well as the Biomedical Ethics Committee, met with the parents to explain Mr. Dunn’s condition and his prognosis. The family was given notice before the Committee hearing and met with the (not at all “nameless” or “faceless”) Committee to discuss their (differing) wants. Thirty days’ worth of medical records, a hospital case worker and assistance in finding alternative care were made available to the family.
Then, there’s the complaint about the limits on visitors and videotaping. It is not unusual to limit Intensive Care Unit visits to specific times and to allow only close family, especially when the patient can’t consent and there is contention among family members. It is certainly standard to prohibit filming in the Unit, since patients are visible from one area to the next, in various states of undress and undergoing constant or frequent *intensive* treatments.
(BTW, one of the lawyers in the TRTL ICU video proves the basis for the rules: he is not compliant with the usual isolation procedures. Former Senator Joe Nixon didn’t wear the protective gown at all correctly, risking the introduction of infectious contamination into the room and/or taking germs home with him.)
It’s very unusual for patients on a ventilator to be conscious because of the severe discomfort associated with the foreign body – the breathing tube – that is necessary in the airways. It’s difficult to believe that anyone would complain about sedating Mr. Dunn in order to bypass his gag reflex.
Finally, the standard of care in advanced metastatic pancreatic cancer is pain relief and palliative support. The surgery to remove a pancreas is extremely dangerous for even healthier patients. As Mr. Dunn had already had an episode of bleeding and both liver and kidney failure, it’s likely that even a biopsy of the pancreatic mass or liver, much less surgery, would have caused more life-threatening bleeding. With liver and kidney damage, he wouldn’t have been able to tolerate trials of radiation or chemotherapy, either.
In fact, the doctors and nurses gave excellent treatment all along, as shown by his survival beyond the average for patients who presented in such a precarious state and acknowledged by Mrs. Kelly in her statement after Chris’ death.
The truth is that Methodist never made plans to “kill” Mr. Dunn. Mr. Dunn was never in danger of the hospital “pulling the plug.” The real problem was a disagreement between Mr. Dunn’s divorced parents over who would legally make medical decisions. That rift is bound to have been made worse by TRTL and the lawyers turning Chris’ illness into a public political battle. The accusations about euthanasia, killing and murder may cause other future patients harm, if they are reluctant to seek care because of these stories.
Sen. Deuell challenges Texas Right to Life over “slanderous” ads | Dallas Morning News
Remember: Senator Bob Duell was instrumental in convincing the medical community to adopt voluntary procedures to protect patients and families affected by the Texas Advance Directive Act, even though actual amendments to the law have been blocked by the very people attacking him.
How much “freedom” does a third party Political Action Committee have in their paid ads? Is it wrong to challenge them legally when the ads are blatantly false?
In this case, the ad opens by implying that Senator Duell is responsible for the too-short 10 day period allowed to find alternate care when the family or patient disagrees with the doctor at the end of life.
Senator Duell was not in the Senate when the Texas Advance Directive Act was passed in 1999. Members of the PAC, Texas Right to Life, were present and lobbied in favor of the Act.
In contrast, Senator Duell has for years been a strong advocate for amendments that would have increased the power of families to protect their loved ones in the case of disputes with the doctor. The amendments would have changed the waiting period to at least a month before any disputed decisions by the doctor would take effect.
As to the challenge, Senator Duell has excellent support for his case:
The Texas Catholic Conference and Catholic Bishops of Texas, who supported Deuell’s bill, have debunked the claims. They said that Texas Right to Life “has tried to stoke fear through ridiculous claims of non-existent death panels and assertions that doctors are secretly trying to kill patients. Both claims are absurd.” The Catholic Conference also ripped Texas Right to Life for spreading “fabrications” about the position of Catholics on the issue.
via Sen. Deuell challenges Texas Right to Life over “slanderous” ads | Dallas Morning News.
Lies, Damned Lies and “ScoreCards”
It takes a long time to write the hard posts, so I’ve been putting this one off for a while. But with Primary season off and running, conservative groups are turning on conservative legislators and using political “score cards” to attack.
Let’s start with the most manipulated “scorecard” of all, especially now that someone else has stepped up to explain so much better than I ever could.
Texas Right to Life, the organization which was criticized by the Texas Catholic Conference for their “misstatements and fabrications” concerning HB303 and HB 1444, continues to make up whatever they wish, this time with their arbitrary “Legislative Scores.” Their scorecard is so “Unconventional” and “perplexing” that it prompted the following letter, signed by all the Texas Catholic Bishops:
December 9, 2013
The Honorable Dan Huberty Texas House of Representatives P.O. Box 2910 Austin, Texas 78768
Dear Representative Huberty:
I am writing at the behest of the Roman Catholic Bishops of Texas to share their concerns about a recent “pro-life scorecard” released by Texas Right to Life (TRTL). This “scorecard” purports to declare which Texas legislators are “pro-life” based on a selective number of votes during the 83rd Legislative Session.
Unfortunately, the unconventional methodology and subjective scoring of the TRTL scorecard produced a number of perplexing results–including assigning low scores to pro-life lawmakers who have worked long and hard to protect and preserve life.
As you know, the Texas Catholic Conference does not use scorecards. Instead, our bishops encourage parishioners to fully form their consciences through prayer and education about issues. Scorecards are a poor substitute for that level of thoughtful policy engagement. Perhaps the most faulty implication of the scorecard is that, in its current form, it casts the tradition of Catholic teaching as being insufficiently pro-life–which is a patently absurd notion. TRTL does not have license to publicly define who is sufficiently pro-life or not.
Some legislative scorecards, when created objectively and appropriately, can be informative. If not, they stop being about informing the public and become more about advancing political agendas, with the unfortunate result that some citizens end up being misled about the issues and misinformed about the voting records of their legislators.
The recent TRTL scorecard selected only three bills (and assorted amendments) to calculate the scores out of the thousands of bills considered during the 83 rd Legislative Session. Several pro-life bills were excluded from consideration. For example, the TRTL scorecard did not include or minimized support for bills that would have prohibited abortion coverage from insurance plans provided in the Affordable Care Act healthcare exchanges (HB 997); prohibited sex selection abortions (HB 309); strengthened parental rights to reduce judicial bypass for teen abortions (HB 3243); or criminalized coerced abortions (HB 3247). All these proposals were unquestionably pro-life, yet were not scored equitably on the TRTL scorecard.
As a result of this selective vote counting, several legislators, who have spent their careerscommitted to pro-life issues, were said to “reject opportunities to protect the sanctity of innocent human life” when that is clearly not the case. For example, Senator Bob Deuell was responsible for requiring abortion facilities to meet the standards of ambulatory surgical centers (SB 537)—a key provision of the landmark prolife legislation that ultimately passed during the Special Session. However, the TRTL political action committee gave him no credit for authoring this pro-life bill. In another instance, State Rep. Bill Callegari was given no credit for his authorship of the parental rights bill (HB 3243).
The method by which the scores were assigned was haphazard and confusing. Some legislators were awarded more points than others for the same legislative action, while other legislators’ contributions were completely ignored. For example, Rep. Jodie Laubenberg and Rep. John Smithee both authored pro-life bills during the session, but Laubenberg was awarded 25 points for authorship of HB 2, while, Smithee was awarded only six points for authoring another pro-life bill that sought to remove abortion coverage in the insurance exchanges. In another example, Rep. Tracey King, who voted against both pro-life omnibus bills (HB 2 and SB 5) received a higher pro-life score than Rep. J. D. Sheffield, who voted FOR both HB 2 and SB 5.
Senator Eddie Lucio Jr. was not scored as pro-life, despite his co-sponsoring and voting for HB 2 and SB 5 and twice crossing party lines to be the final necessary vote to suspend Senate rules and debate on these bills.
What was most troubling to the Texas Catholic Bishops was that the scorecard appears to attack those legislators who supported perhaps one of the most pro-life bills during the 83rd session: protecting individuals and families at the end of life by reforming the Texas Advance Directives Act. Advance directives reform not only would have given families more tools to protect their loved ones at the end of life, but would have provided conscience protections to medical providers to refuse inflicting burdensome and unnecessary procedures on patients. The advance directives law would have changed current law to:
prohibit the involuntary denial of care to critically ill patients, including food and water;
prevent doctors from making unilateral “Do Not Attempt Resuscitation” orders without consulting families; and,
require treating all patients “equally without regard to permanent physical or mental disabilities, age, gender, ethnic background, or financial or insurance status.”
The advance directives reform bill was a moral and compassionate approach to end-of-life care that was opposed by TRTL, but supported by a broad coalition of groups, including the Texas Catholic Conference, the Texas Baptist Christian Life Commission, the Texas Alliance for Life, the Coalition of Texans with Disabilities, the AARP, the Texas Pro-Life Action Team, the Texas Conservative Coalition, and the Catholic Hospital Association of Texas. Advance directives reform was important to the Catholic Church–and to many legislators–because we recognize human life as a gift from God that is innately sacred–from conception to natural death. We have taken this position after much reflection to ensure that the law respects the natural dying process.
The implication to be drawn from this scorecard is that TRTL opposed the advance directives reform bill, and appears to have taken to punishing those pro-life legislators who disagreed with them by inaccurately casting them as not being sufficiently pro-life. That is plainly inaccurate.
In the case of the advance directives reform bill, legislators who supported the law were strongly pro-life; they merely opposed the TRTL’s position. These are not necessarily the same thing. It is unfortunate that so many members who continue to fully stand for life are being attacked for doing just that. We hope that this letter has clarified what would otherwise have remained an unfair and confusing characterization.
Sincerely,
Jeffery R. Patterson Executive Director
NEJM “I want” ethics
In the Abolition of Man, C.S. Lewis notes that, “When all that says ‘it is good’ has been debunked, what says ‘I want’ remains.”
Last week, the New England Journal of Medicine published a “Perspectives” column, “Life or Death for the Dead Donor’s Rule?,” in which the authors illustrate Lewis’ point with their redefinition of non-maleficence to better serve a re-defined autonomy.
They would convince us that there is no harm in hastening the death of a dying patient even by intentionally causing it if he or his surrogates ask. They ignore a 2500 year old First Principle of Medical ethics,focused on the health of the patient in front of us: “Cure when possible, but first do no harm, ”
Autonomy, like all rights, is a negative right: the patient has the right to refuse invasive medical interventions that will harm him or that he does not want. Patients and surrogates, if they can compel the use of medical skills and invasive technology, can only do so for the medical benefit of the patient himself.
Illogically, in these times of reducing costs, the authors would have us consider taking a patient from the ICU to the OR “and then take him back to where life support would be withdrawn.” The return to the ICU is nothing but our own “medical charade.”
The Abolition of Man can be read online, here, or you can buy the Kindle version at Amazon.com.
I want to thank Nancy Valko, who runs an email list covering a range of traditional ethics issues, her email alerting me to this editorial.
“Choosing Wisely: Five Things Physicians and Patients Should Question”
 Bookmark this page: “Choosing Wisely: Lists.”
Bookmark this page: “Choosing Wisely: Lists.”
Whether you are seeing your doctor for a cold, a routine physical or a “new patient visit,” or when you suspect that he’s offering you the famous notorious “blue pill or red pill,” how do you as a layman know whether a medical test or procedure is needed? Will it lead to a treatment decision or just more tests? Does it help? Or does it actually cause harm?
Or politically, will ObamaCare cost cuts and rationing deny you a procedure, test, or treatment that would be helpful?
The American Board of Internal Medicine Foundation asked the various physician sub-specialty organizations in the US to list tests, treatments and procedures that don’t help or might actually hurt patients. The lists are published on the “Choosing Wisely” website.
Remember, there’s a difference between screening tests that look for something you might have, and diagnostic tests to explain a symptom from your history or chief complaint, a finding on an exam or to determine whether a treatment is working or harming. And there’s certainly a difference between starting a treatment, doing a procedure or ordering a test that leads to more risk than the disease or condition we’re treating just because . . . of money, out-of-date knowledge, or patient desire. Or because we can.
Whatever health care problem or concern you have, take a look at the list from the medical specialty for the pertinent body part or organ system. Which tests and procedure do you need, and which have you had that are on these lists?
I don’t quite agree with all the items on all the lists. After all, patient care is not a recipe from a given cookbook – and besides, patients’ bodies can’t read the books to follow the recipes.
Let’s talk! Ask me questions and/or let me translate the jargon.
Texas or DC: Who do you want regulating your doctor?
Peggy Fikac once again proves that she’s not a reporter, and most certainly not anything like a fair and balanced media representative.
From the Houston Chronicle’s coverage of events in Austin, today:
“Obamacare is the wrong prescription for American health care, and I will never stop fighting against it,” Abbott said, joined by small business people and a doctor who also oppose the law at a company, the Texas Mailhouse.
One reason that Abbott gave for fighting the law came in response to a doctor who asked him from the audience about what Texas could do to keep the federal law from interfering with doctors’ judgment about the best way to treat their patients.
“You’re raising one of the more challenging components of Obamacare, and a hidden component in a way, and that is government is stepping in between the doctor-patient relationship and trying to tell you what you can and cannot do, interfering with both your conscience and your medical oath to take care of your patient,” said Abbott, who is campaigning to succeed Gov. Rick Perry.
That is similar to arguments raised against tighter abortion restrictions approved in special session, including a ban on the procedure at 20 weeks, along with stricter regulations on clinics and abortion-inducing drugs.
I am that doctor from the audience. Ms. Fikac is correct that I voiced concern over the Federal interference between the patient and the doctor. She’s flat wrong about Texas regulation of medicine by bring abortionists up to standards being equivalent to the
I prefaced the question by noting that it is the State of Texas that properly regulates Texas Doctors and medicine. At the State level, patients and doctors have more influence on our elected officials and the people they appoint to write regulations and enforce the law than we do on the Federal level.
I also noted that because of the increasing interference over the years by Medicare, I am concerned about the reach that this new set of regulations will have, including ever-invasive micro-reporting of patient’s private medical conditions. (I named the upcoming move to the ICD-10, which will be a nightmare, requiring doctors to make distinctions between medical conditions, out to five (5) decimal places.
As bad as the bureaucracy of the Office of the Inspector General for the Federal Health and Human Services and the Centers for Medicare and Medicaid Services have been in the past, I don’t look forward to the additional layer of IRS income verification, audits and enforcement.
We could stick closer to home, with the Texas Health and Human Services, the Texas Medical Board, and the Texas Insurance Commission!
Denouement: The Death of #SB303
The 83rd Legislature of the State of Texas still has a couple of weeks to go, and it ain’t over ’till both the House and Senate are sine die, but it appears that SB 303 did die over the weekend.
Representative Susan King, who broke her leg last Sunday, just the day before the marathon meeting of the House Public Health Committee, has done an incredible job of working with Senator (Dr.) Bob Duell in their attempt to reform our State’s Advance Directive Act through SB 303.
The Committee Substitute which Representative King presented in the Committee had all of the benefits I wrote about last week, as well as a revision to prohibit a doctor from writing a DNR order against the wishes off a competent patient.
(Talk about unintended consequences: current law is silent on “DNRs,” so it’s apparently legal for a doctor to order that resuscitation not be performed on a competent patient without any discussion with the patient, much less obtain consent! I have sincere doubts that any doctor would do so, but there have been allegations. Even though the ones who claim to have knowledge – and who have not produced one iota of proof – are the same disingenuous cynical scaremongers (I’ll call them “CS2”) I’ve mentioned before, this reform would be a good. And should be accepted on its face.)
Because of the egregious misrepresentations of the CS2, Committee Chair Lois Kolkhorst declined to allow SB303 out of the Committee as it was written. Rep. King tried one more time, with a bare bones CS1 containing the protection against DNRs for competent patients and the prohibition against withdrawal of Artificial Hydration and Nutrition, except when it would harm the patient or hasten his death.
So, for the next two years, when you hear the CS2 complain about Texas “death panels” or read a plea for funds to fight “secret DNRs” and withdrawal of food and water in Texas hospitals, remember the CS2 who killed pro-life reform in the 83rd Legislature.
My Testimony on #SB303 (Conscience, Rights, Medical Judgment and Law)
Note: I’ve heard that there’s a new Committee Substitute that will soon be introduced that is more explicit on DNR’s, especially on informed consent and on competent patients.
If laws demand that physicians perform acts against our consciences, you will end up with only doctors without consciences willing to perform the acts in question.
After a few more words about the meeting of the 83rd Texas Legislature Public Health Committee, I’ll post my written testimony that I turned in to the Committee. You can watch the video of the meeting, here. My testimony begins about 4:59/8:20.
I spoke just before midnight, after many others had covered the good (or bad, depending on their opinions) reforms in SB 303, so I didn’t really go in to those when I talked. Instead, I explained how I handled the few times I’ve had to write DNR’s without consent from the patient or a surrogate.
I also talked about the medical judgement of physicians, about the definition of the “right to life”as a negative right. This means that I can be prohibited from killing, but not that I can be forced to indefinitely act against my conscience and medical judgment. It’s a tough concept, meaning no one can claim that their right to life means that they can take my food and shelter, my labors or my liberty to keep them alive.
Then, I explained that yes, doctors have a special relationship, a covenant or, at least, a professional relationship due to our privilege of practicing medicine. But the duties aren’t unlimited and they are not all one way. The 10 days plus 21 days in the version of SB303 that we were discussing that night should be a sufficient time trial or test of time for the patient and the doctor’s decisions about the medical treatment, including DNR’s, that the family demands.
The explanation about the nature of medical judgment that I gave is in the written testimony:
May 13, 2013
Chair Kolkhorst and members,
The Texas Advance Directive Act of 1999, created a procedure for resolving disagreements between doctors and their patients or surrogates about which interventions are medically appropriate. The experiences of patients and doctors during the few times that procedure has been invoked over the years, revealed some problems.
The reforms in SB 303 improve the Advance Directive Act by
· Giving patients and their surrogates much more time and assistance than current law provides in order to prepare for the ethics committee meeting and, if necessary, to find a new doctor willing to accept responsibility for the care of the patient,
· Clarifying the succession of surrogates under state law,
· Protecting the patient’s access to artificially administered hydration and nutrition,
· Restating Texan’s belief that patients should be treated equally regardless of age, disability or ability to pay,
· Adding a whole new section regulating the implementation of Do Not Attempt Resuscitation orders, which our State law hasn’t addressed at all in the past, and
· By protecting the conscience rights of doctors from undue threat of civil, criminal and regulatory liability.
After all, while the hospital provides structure in the form of policies and the medical committee provides oversight about ethics and standard of care, it’s doctors like me, not hospitals or committees, who practice medicine using our medical education and experience guided by conscience, or medical judgment. Medical judgment, not lawyers and paperwork at the bedside, is what enables me to predict the effectiveness of interventions before I order them.
Like all but a handful of Texas doctors, I’ve never had to ask for a medical ethics committee review, but I have had to ask another doctor to co-sign a DNR when I couldn’t find a legal surrogate. As a family doctor, I’ve found that algorithms and “cookbook medicine” or lines of succession for absent family members sometimes aren’t enough when a patient’s physical condition is deteriorating quickly or even when disease runs its expected course, causing organ system after organ system to fail.
Ethics and laws generally lag behind medical advances. Once upon a time, people who couldn’t breathe for themselves were considered to have died a “natural death,” but we keep changing the rules about what we expect human bodies and the “art” of medicine to do. Please support the necessary and important reforms in SB 303.
Thank you for your time and attention,
Beverly B. Nuckols, MD, FAAFP, MA (Bioethics)
Public Health Hearing on #SB303
Last night, an emergency meeting ot the 83rd Texas Legislature’s Public Health Committee addressed Senate Bill 303, by Senator Duell in a 12 hour long meeting. Representative Susan King, who authored the Companion Bill in the House and sponsored SB303 in this meeting, appeared only one day after a fracture of her tibia. This woman is a hero!
I also want to thank Chair Lois Kolkhorst for ensuring that the meeting was held so that SB303 – and all the people who are so passionate about patients rights and good medicine in Texas could be heard.
It was wonderful to see all the people who volunteer so much of their time to influence Texas law – even when they disagreed with me. What a pleasure to meet new friends, including a gentleman whose name I can’t recall (will fix this later) and Jacqueline Harvey, Ph.D.
Here’s an excerpt from Dr. Harvey’s testimony,
While opponents say that S.B.303 grants power to providers to remove care patients in irreversible conditions, I’d remind them again that one cannot extend to providers power which they already legally possess. Opponents claim that S.B. 303 adds this broad definition, when in fact; this broad definition was established in TADA and is current Texas Law. What S.B. 303 does is add protections to prohibit discrimination against persons with disabilities by ensuring that care may be removed only when harmful (i.e. treatment would fail, hasten patient death, exacerbate another medical condition or cause unnecessary pain). These conditions are standard medical ethics a la “do no harm.”
I’ll write more after I get a chance to review the video of the hearing. There’s some sort of glitch at the Legislature Audio and Video page. (Might have something to do with 12 hours of recordings, ending after 2 AM)