WingRight
Medical ethics
Maternal Morbidity with Premature Rupture of Membranes <24 Weeks
Because of the recent Supreme Court ruling, Dobbs vs. Jackson Women’s Health Organization, that overturned Roe v. Wade, misinformation has been spreading online and in public forums about the risk of maternal morbidity and mortality to mothers after premature rupture of membranes at less than 24 weeks or in the second trimester, which occurs in 0.3% to 0.4% of all pregnancies. The misinformation infllates the risk and usually tells of doctors’ hesitancy to treat due to fears of legal consequences.
In April, 2022, the American Journal of Obstetrics and Gynecology (AJOG) published an article, “Maternal morbidity after preterm premature rupture of membranes at <24 weeks’ gestation,” by Sklar A, Sheeder J, Davis AR, et al.
On average, there’s a greater risk in watch & wait. A day or 2 of careful conservative observation is much different than 14 days.
If you’re interested, here’s my review of the article Free! It costs $39 to read this whole thing, if not a subscriber.
We knew the risk difference for later gestations from past research. There have been a few studies describing the risks of maternal morbidity from premature spontaneous rupture of membranes (PROM) before 24 weeks, but the numbers were small & excluded women who chose termination of pregnancy.
In this retrospective cohort study – a chart review – from 2011 to 2018 at 3 hospitals, the review of 350 charts were randomly selected from an original 6747 potential cases to include. Of that 350, 208 were eligible, with women who spontaneously delivered within 24 hours excluded from the study, along with women with chorioamnionitis on initial presentation, fetal abnormalities, or PPROM after an invasive uterine procedure like amniocentesis.
Women who chose exprctant management (EM) but later decided to terminate the pregnancy were counted with the EM group.
Both induction of labor and d&e were included in the termination of pregnancy (TOP) cohort. Although the article describes the difference in the possibility of fetal survival, the outcomes were combined. This was noted as a weaknes in the article.
[My note: The prep for the induction is either a 1-2 day outpatient process for the d&e (with symptoms much like early labor), or an emergency manual dilation in the OR (with shorter preps having more risk to the integrity of the cervix).]
51.9%, 108 women, chose EM & those tended to be farther along in their pregnancies (mean gestational age 21 6/7 weeks vs 18 6/7).
2/3 of the TOP were labor induction & 1/3 d&e.
42 babies, 38%, of the 108 EM, survived to discharge. 15% of these mothers had no maternal morbidity, 37% of the group had both fetal demise & maternal morbidity. Composite morbidity was 60%.
All of the 100 TOP fetuses died. Maternal morbidity was 33%.
Counterintuitive abortion report
Legalize arbitrary homicide to decrease arbitrary homicide? Talk about counterintuitive!
I enjoy debating bioethics and politics online because it encourages me to think, research and tighten my arguments. I spend at least part of each day explaining and advocating for the protection of human rights, especially the right to life, or the right not to be killed. I’m not only trying to convince the people engaged in the conversation, but the “lurkers” who read but don’t post.
I endeavor to read and evaluate as many as possible of the sources and references that are used to counter my arguments. I learn and hope to be a better debater that way.
During an one such debate, I was referred to a 2020 article in the journal Lancet, “Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019,” that supposedly gave proof that abortion restrictions result in higher rates of abortion.
The report proves that statistics can be manipulated based on estimates which are actually Wild-Assed Guesses. Working from an estimated 73.3 million abortions per year worldwide, the authors admit that virtually all of the data are “estimates” rather than actual numbers.
But, to strengthen their model, they threw out 62% of women at reproductive age because data from China & India, where abortion is broadly legal, “skewed” their numbers.
Besides the fact that it would be useful to know how they determine the number of illegal abortions in a country, the “findings” are reported by region & broad income. (And in a cluttered pdf at https://www.thelancet.com/cms/10.1016/S2214-109X(20)30315-6/attachment/d4652ad7-9ace-425e-b907-7060ff71982f/mmc1.pdf )
Look at the Caribbean countries where countries with just about every possible combination of restrictions & income level are lumped together. ( And Cuba is reported as upper middle income.)

Which might or might not explain,
…..
“Among middle-income and low-income countries, there was not a clear relationship between legal restrictions and abortion rates, or the proportion of unintended pregnancies ending in abortion.”
And,
“2015–19, low-income countries had the highest unintended pregnancy rate and the lowest proportion of unintended pregnancies ending in abortion.”
If we accept the WAG numbers that the authors admit are higher than those of other researchers, there is an indication that lower income regions have more pregnancies the authors categorize as “unintended.” And, if a country starts out at an abortion rate of 30, increasing to 39 gives a higher percentage change than countries that start at 61 & go to 70.

At least the headings in the Summary are semi-truthful: “findings” & “Interpretation.” But the data doesn’t indicate that restrictions result in more abortions.
Comprehensive review of Texas’ Heartbeat Act
Excellent, thorough, and true! Since I could never do better and can’t imagine editing, I’ve been given permission to copy & paste. Please give it your time and attention!
(The group is an excellent source & great to follow on Twitter, @secularprolife)
Secular Pro-Life Perspectives
Wednesday, September 29, 2021
The Texas Heartbeat Act: Answers to 11 Frequently-Asked Questions
Today’s guest post is by Daniel Gump.
After passage of the Texas Heartbeat Act (Senate Bill 8), numerous misinformation campaigns have led to confusion among the general public as to what the legislation covers and how violations are handled. Because of this, I have encountered several of the same questions and inaccurate statements repeated on social media over the past couple months. The following responses address some of these questions.
1. What is excluded from the definition of “abortion”?
Health and Safety Code already defines abortions under Sec. 245.002, and the Act did not amend them. Subsection (1) states:
(1) “Abortion” means the act of using or prescribing an instrument, a drug, a medicine, or any other substance, device, or means with the intent to cause the death of an unborn child of a woman known to be pregnant. The term does not include birth control devices or oral contraceptives. An act is not an abortion if the act is done with the intent to:
(A) save the life or preserve the health of an unborn child;
(B) remove a dead, unborn child whose death was caused by spontaneous abortion; or
(C) remove an ectopic pregnancy.
This definition is similar to those across the entire United States, as treatment for ectopic pregnancies and post-miscarriage treatment are not criminal acts in any jurisdiction. The laws solely address intentional acts of feticide.
2. How are medical emergencies handled?
The legislation declares for Health and Safety Code §171.203-§171.205 that abortions performed or induced for legitimate medical emergencies are exempted from prosecution. They must be logged in the woman’s medical records and retained in the physician’s own practice records.
The existing Sec. 171.002 defines what would be considered a medical emergency:
(3) “Medical emergency” means a life-threatening physical condition aggravated by, caused by, or arising from a pregnancy that, as certified by a physician, places the woman in danger of death or a serious risk of substantial impairment of a major bodily function unless an abortion is performed.
3. How are fetal anomalies addressed?
The Texas Heartbeat Act is silent on fetal anomalies of any type, so an unborn child with Down syndrome, spina bifida, hydrocephalus, or other conditions is protected from abortion, unless the pregnant woman’s life is in danger.
4. Could women be sued for procuring abortions in Texas?
No, Section 3 of the Act adds Sec. 171.206 to the Health and Safety Code. This includes the text:
(b) This subchapter may not be construed to:
(1) authorize the initiation of a cause of action against or the prosecution of a woman on whom an abortion is performed or induced or attempted to be performed or induced in violation of this subchapter;
(2) wholly or partly repeal, either expressly or by implication, any other statute that regulates or prohibits abortion, including Chapter 6-1/2, Title 71, Revised Statutes;
Several other statutes already protect women from criminal abortion liability. Examples within the same code Chapter 171 include:
Sec. 171.064. ADMINISTRATIVE PENALTY.
(b) A penalty may not be assessed under this section against a pregnant woman who receives a medical abortion.
Sec. 171.106. APPLICABILITY.
A woman on whom a partial-birth abortion is performed or attempted in violation of this subchapter may not be prosecuted under this subchapter or for conspiracy to commit a violation of this subchapter.
Sec. 171.152. DISMEMBERMENT ABORTIONS PROHIBITED.
(b) A woman on whom a dismemberment abortion is performed, an employee or agent acting under the direction of a physician who performs a dismemberment abortion, or a person who fills a prescription or provides equipment used in a dismemberment abortion does not violate Subsection (a).
Sec. 171.154. CONSTRUCTION OF SUBCHAPTER.
(d) This subchapter may not be construed to:
(1) authorize the prosecution of or a cause of action to be brought against a woman on whom an abortion is performed or induced in violation of this subchapter;
5. Could women be sued or held liable for leaving Texas to procure abortions in another state or country?
There would be no civil or criminal liabilities within Texas for women receiving abortions, so any such liabilities would fall under the jurisdictions where the abortions take place. Holding women liable for abortions is very rare in any nations following English common law (as the US does when no statutory law exists to the contrary).
Of all 50 states, the only ones that explicitly allow for women to be criminally liable for abortions are:
- Delaware (11 Del. Code §652) – Class A misdemeanor (past viability)
- Nevada (Nev. Rev. Stat. §200.220) – Manslaughter (past 24wk)
- Oklahoma (21 Okla. Stat. Cit. §652(E), §691(D), §713(C)) – Manslaughter (if during commission of another crime)
- Utah (Utah Code §76-5-201) – Women only exempted from homicide laws in regards to legal abortions or unintentional actions.
6. Could taxi drivers and rideshare drivers be liable for transporting women to receive abortions?
This would take a very liberal interpretation of the new Sec. 171.208(a) to include drivers under “any person who…”
- performs or induces an abortion in violation of this subchapter;
- knowingly engages in conduct that aids or abets the performance or inducement of an abortion, including paying for or reimbursing the costs of an abortion through insurance or otherwise, if the abortion is performed or induced in violation of this subchapter, regardless of whether the person knew or should have known that the abortion would be performed or induced in violation of this subchapter
- intends to engage in the conduct described by Subdivision (1) or (2).
Drivers are multiple degrees separated from (2) aiding or abetting “performance or inducement” of abortions, and they are not (3) intending such action by transporting customers between locations.
The claim that drivers would be liable was little more than a publicity stunt by Lyft to inject themselves into discussion on the legislation. In their press release, they were very careful to avoid use of the word “abortion” and repeatedly hid behind euphemisns like “healthcare they need,” “healthcare appointment,” “healthcare access,” etc. This made the Texas Heartbeat Act seem like its purpose was to block women from seeing their OB/GYNs or other healthcare practitioners.
Lyft also made it clear that drivers and riders should follow a don’t-ask-don’t-tell policy for any illegal activities. The press release closed out with an announcement of a legal defense fund for drivers ferrying women in violation of the Texas Heartbeat Act, a $1 million donation to Planned Parenthood, and a link (with tracking parameters in the URL) for individuals to further donate to Planned Parenthood.
7. Could the rapist of a woman receiving an abortion sue the physician or anyone else involved for $10,000?
No, Section 3 of the Act adds Sec. 171.208(j) to the Health and Safety Code that states:
Notwithstanding any other law, a civil action under this section may not be brought by a person who impregnated the abortion patient through an act of rape, sexual assault, incest, or any other act prohibited by Sections 22.011, 22.021, or 25.02, Penal Code.
The Penal Code sections referenced address “Sexual Assault,” “Aggravated Sexual Assault,” and “Prohibited Sexual Conduct,” respectively.
8. Can anyone claim “bounty” after an abortion is performed?
What makes the Texas Heartbeat Act unique among fetal heartbeat legislation is that it declares any non-government individual to have standing to sue. The claims of open bounty on abortion clinics are exaggerated, as generally only those close enough to the acts would have enough evidence to merit lawsuits. Presumably, those close enough would include the women who had the abortions, the father of the unborn children, any relatives or guardians of either, and possibly those within their inner circles.
A random individual would have difficulty presenting a strong case, particularly with HIPAA laws and Texas’ own privacy laws concerning abortion reporting under Chapter 171 of the Health and Safety Codes. Any individual performing or inducing abortions who provides enough details to the general public about specific violations would likely be in violation of several other laws, as well.
Any lawsuit would also have to follow established legal procedures in the state under the Civil Practice and Remedies Code, Code of Criminal Procedure, and any other applicable areas of the Revised Statutes. A state-wide free-for-all to claim $10,000 per violation is not likely, as a claimant would have to pay court fees and attorney fees on a lawsuit with dubious chance of actually succeeding. Plus, an award is only available once per violation (Sec. 171.208(c)).
On September 18, 2021, abortionist Alan Braid wrote an article for The Washington Post in which he admitted to violating the law. He was careful to avoid publicly disclosing specific details, but two individuals residing out of state (Oscar Stilley and Felipe N Gomez), nevertheless, filed lawsuits against him to test the law. As these cases are still pending, their merits are difficult to determine.
9. What method must be used to determine the fetal heartbeat?
Section 3 of the Act adds Sec. 171.203 to the Health and Safety Code, which describes the means as being “standard medical practice”:
(a) For the purposes of determining the presence of a fetal heartbeat under this section, “standard medical practice” includes employing the appropriate means of detecting the heartbeat based on the estimated gestational age of the unborn child and the condition of the woman and her pregnancy.
(b) Except as provided by Section 171.205, a physician may not knowingly perform or induce an abortion on a pregnant woman unless the physician has determined, in accordance with this section, whether the woman’s unborn child has a detectable fetal heartbeat.
(c) In making a determination under Subsection (b), the physician must use a test that is:
(1) consistent with the physician’s good faith and reasonable understanding of standard medical practice; and
(2) appropriate for the estimated gestational age of the unborn child and the condition of the pregnant woman and her pregnancy.
Any specific requirements for methods fall outside the scope of the legislation and within any medical licensing boards of medical associations.
10. How far into pregnancy does the abortion ban take effect?
Based upon the definitions in the new Health and Safety Code Sec. 171.201, there is no specific time period, as the ban is based upon the ability to detect a fetal heartbeat, using “standard medical practice.” From subsection 1:
“Fetal heartbeat” specifically means cardiac activity or the steady and repetitive rhythmic contraction of the fetal heart within the gestational sac.
Even though the term used is “fetal heartbeat,” the scope of the law includes embryos, based on subsection 7:
“Unborn child” means a human fetus or embryo in any stage of gestation from fertilization until birth.
The actual method of detecting the heartbeat of the embryo or fetus relies on the discretion of the one conducting the test.
Johns Hopkins Medicine states that a transvaginal ultrasound can detect the heartbeat by 5-6 weeks, and an abdominal ultrasound can detect one by 7-8 weeks. These are just estimates that can depend on a number of circumstances, like quality of equipment and training of the individual.
Sec. 171.203 requires a physician to record the method of detecting the fetal heartbeat and the estimated gestational age. Presumably, this would reduce purposeful attempts of deceit to circumvent the law.
11. Did the Texas legislature increase funding to social programs within the Texas Heartbeat Act?
Though not part of the same legislation, the state’s budget increased several social programs for the year.
The “Alternatives to Abortion” program under the Texas Health and Human Services has seen a budget increase every two years since its inception. For the 2022-2023 biennial budget earlier this year, there was a 25% increase from $80 million to $100 million. This program addresses financial and material needs of pregnant women and parents. The website lists examples of services:
- Counseling, mentoring, educational information and classes on pregnancy, parenting, adoption, life skills and employment readiness.
- Material assistance, such as car seats, clothing, diapers and formula.
- Care coordination through referrals to government assistance programs and other social services programs.
- Call center for information and appointment scheduling.
- Housing and support services through maternity homes.
Additionally, the budget increased the following:
- $135.5 million for various mental health programs
- $10.2 million for women’s health programs
- $123.5 million for rural hospitals
- $164.2 million relating to foster care
- $57.6 million for combatting human trafficking

Photo by Matt Walsh from Unsplash
Powered by Blogger.
Candace Owen’s rant
I usually agree with Candace, but this video that’s circulating is propaganda and over the top. I won’t embed the video but you can go waste 30 minutes if you want, at this Facebook page.
I listened to 27 minutes. She gets to employer’s around 20 minutes in.
She has some things right, others very wrong.
Right:
A. Yes, social media is wrong to censor doctors.
B. Yes, vaccines should be voluntary.
Wrong:
- She’s conflating an acute asthma attack with a prophylactic vaccine for healthy people.
- Where’s the evidence that the US government is even telling, much less pressuring private employers? (*That* would be “communism,” or socialism, if government controls business.)
- There’s approval by the FDA. It’s emergency approval, but approval, just the same.
- Well over half of the US – 55% – has had at least one shot. 49% fully vaccinated over the age of 12. 59% of those over the age of 18. 200 million people in the US alone is a significant trial. We’re way beyond the “experimental” stage, with millions of life-years of evidence.
- And, for my British Virgin Island friends, The BVI isn’t the US.
Now, as to the employers…
Do business owners have no say in who they employ or the conditions of employment? Does the government own the business, so can make company policy? Do business owners answer to customers or their employees?
I don’t agree with mandatory vaccination if government does the forcing. And employers should use their policies wisely and carefully, only requiring legal, safe, and ethical acts from their employees.
The vaccine is legal, safe, and ethical.
Unlike government mandates, a business owner doesn’t use threats of guns and prisons. He sets company policy. If employees don’t like it, they aren’t slaves or indentured servants who must stay & follow the rules. They can leave.
No one owns their job. No one owes them a job.
Arguments?
Normal & reality: a proposed definition for discussion
On one of the Facebook groups I follow, the conversation about the recent Arkansas law protecting conscience was diverted from the law itself by a sensational headline that reflected only the worst accusations of opponents & the reactions of group members to that headline.
During the conversation, I was questioned about my use of the term “normal” for healthy bodily functions. At the least, “normal” is that which doesn’t itself injure tissues & organs and doesn’t require technological intervention to produce or to prevent morbidity & mortality.
We are hearing & reading about demands that legitimate research results should be suppressed, watching physicians and scientists who express heterodox opinions be censored. Then we’re told that there’s a “consensus,” since none of the “objectionable” research is published, much less popularized, and the outliers are demonetized and covered with warning boxes.
Science isn’t a “consensus.” In science, true hypotheses are testable, with valid results capable of being confirmed by different observers under similar conditions in different labs.
That’s also a good definition of reality or “normal.” One that could be applicable to medical subjects like COVID or vaccines, as well as social and legal matters.
We’re being manipulated for reasons that have nothing to do with actual health, physical or mental. I can’t fathom a reasonable explanation. It looks like an exertion of power – social, financial, then legal.
Patients won’t be helped at all by forcing moral injury by requiring medical professionals to act against their conscience and we all lose when rational discussion is suppressed in the public sphere.
South Africa COVID Variant and the AstraZeneca Vaccine
CNN & NYT coverage of events in South Africa concerning the AstraZeneca vaccine that’s being given in the British Virgin Islands are very poor.
The new study doesn’t come out until today, so the “news” reports are based only on press releases.
ONE variant. ONE country.
And the actual data isn’t even available yet, even as preliminary information…
From what is available information in these reports about South Africa: About 1500 young people, average age 31, were studied in South Africa, half received the vaccine, half a placebo. This study only evaluated one strain, and only mild to moderate infections, because this age group doesn’t tend to get sick.
All we really know is that in the South Africa study, similar numbers became infected with that particular strain and the serum from their blood didn’t do a good job of neutralizing that strain in the lab.
From the BBC news reports:
“Data from the Oxford-AstraZeneca vaccine team suggests their vaccine protects just as well against the new UK variant, but offers less protection against the South Africa variant – although it should still protect against severe Covid-19 illness.”
The vaccine *does* have high efficacy protection for the older strains & the UK variant. Not only that, but if vaccinated, the infectious period is shorter for these varieties.
There’s evidently no safety concern about the AstraZeneca vaccine from either study.
Beverly B Nuckols, MD
Scott Atlas, MD, in his own words
You’ve probably heard about the new doctor, Scott Atlas, MD who is advising President Trump on health policy during the last couple of months.
Here’s a video in which he describes his views and recommfations. You might be surprised!
Dueling Statements by “Experts:” More COVID-19 politics
About the “Born-Alive” Debate
For those interested in the Born Alive issue, here’s a “pro-choice” leaning “FactCheck.org” article that generally has the details right. It’s the conclusion that is flawed.
We don’t know the specifics of President Trump’s Executive Order, but there’s quite a bit of controversy in social media and the news media.
The Fact Check article claims that neither the 2002 Act nor the 2019 (failed) Bill are necessary due to homicide laws in the States as well as Federal law.
However, there has always been a very real debate about both the babies on the cusp of viability and babies born alive in the process of an induced abortion.
The latter was addressed in the 2019 Bill that failed to pass. Specifically, that Bill (would have) mandated standard of care medical attention.
A modest proposal for COVID-19 response (Or, I’m not King, but)
If I were in charge of the public health response to COVID-19, I would implement the following:
Pharmacy Boards should never get between a doctor and patient except in matters of life and death or illegal practice. Politicians, State Medical Boards and our House of Medicine professional organizations should defend our legal practice of medicine rather than threatening physicians and changing the rules during a pandemic.
2. Encourage shared information & fact-checking among physicians as part of our missions of education & transparency.
JAMA review of masks, August 2020
4. Where a high percentage of the local population tests positive, local authorities should consider – and have the ethical responsibility to – impose higher isolation measures like masks and public distancing. The threshold for mandates must be locally determined with public input, and explained – clearly, frequently.
This means you, anti-maskers!
5. Stress that surgical procedure masks are nearly as effective as N95 masks, blocking nearly as much aerosols and viral particles for both wearer and those around us. Medical providers and those with a high risk of prolonged close contact need fitted N95 masks, the rest of us don’t.
Single layer cut-up T-shirts and homemade masks, balaclavas or bandannas, aren’t very effective protection at all, either for the wearer or the people around us. N95 Masks with single valves are a money-maker, but not nearly as effective as surgical masks, even with an added filter layer.
8. Begin early prophylaxis with hydroxychloroquine/zinc and/or inhaled steroids for the willing & likely exposed.
REFERENCES
Treatment dosing (always allowing treating physicians who prescribe determine need & frequency of alternate doses & monitoring)
This isn’t a prescription!
Hydroxychloroquine: 400 mg. twice on day one then 200 mg. twice a day for either 5 or 10 days;
Azithromycin: 250 mg. tablet, 2 on day one, 1 on day 2 to 5;
Budesonide: unit dose via hand held inhaler or nebulizer twice a day. (I’m looking for references for this one. )
Zinc 150 mg. to 250 mg. a day indefinitely. (Best evidence for lozenges or syrup multiple times a day. See references.)
Vitamin D, 1000 IU a day, up to 4000 IU is safe
Vitamin C, No set dose, but extra will be excreted in the urine or feces, can cause diarrhea.
References
Journal of the American Medical Association review. Published August 11, 2020. (Free, with Tables)
CDC recommendation on cloth masks:
https://wwwnc.cdc.gov/eid/article/26/10/20-0948_article
John’s Hopkins recommendation:
Zinc:
https://www.uchealth.org/today/zinc-could-help-diminish-extent-of-covid-19/
Journal article on treatment for the common cold: https://www.acpjournals.org/doi/10.7326/0003-4819-125-2-199607150-00001
Hydroxychloroquine/azithromycin protocols
International Journal of Infectious Diseases (Henry Ford or Ashad report):
https://www.ijidonline.com/article/S1201-9712(20)30534-8/fulltext
https://www.ijidonline.com/article/S1201-9712(20)30600-7/fulltext
On synergistic effect of hydroxychloroquine plus steroids:
https://www.ijidonline.com/article/S1201-9712(20)30613-5/fulltext
Budesonide
Description of study in progress on treatment for loss of smell in patients without severe symptoms:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7370627/
Vitamin C safety:
Note: comments are off. Please comment on my Facebook page, Beverly Nuckols.
Edited 31/08/20 12:30 for mis-spellchecked word. BBN
Consult this (Dr.) Atlas

Dr. Scott W. Atlas, former Chief of Neuroradiology at Stanford University Medical Center, current Senior Fellow at Stanford’s Hoover Institute, author, and public health policy consultant was added to the White House COVID-19 task force this week. Unfortunately, he and his appointment have already become a political target by some.
Far from being unqualified, or someone who “clearly wouldn’t know science if it kicked him in the atlas” (see above link – I refuse to give clicks to the original source or the ignorant woman who spoke those words), Dr. Atlas speaks common sense, science-based truth, as in this video from 23 June, 2020 interview with Peter Robinson of the Hoover Institute’s. “Uncommon Knowledge.”
In fact, Dr. Atlas states what I’ve been saying since I heard about the virus outbreak in Italy, while attending Carnivale parades just a few miles away in

Carnivale float, Nice France, depicting Chinese labor in Fashion industry.
Nice, France: the reaction by governments and fearful people has been just as bad if not worse than the results of the infection itself.
The initial lockdown was correct, but we have new data – and new models – every day. Yet, we are still acting as though the early models were accurate.
Worse, instead of “flattening the curve,” the call is to conquer or eliminate the virus “at all costs.” The latter has never happened and will never happen with a Coronavirus. There is the possible exception of the elimination of smallpox, a much more deadly disease, at the cost of egregious human rights violations and even deaths.
I’m surprised that anyone would attack Dr. Atlas or his qualifications. Before you dismiss him, please listen to his testimony and critique the facts rather than the source.
Interview with Dr. Immanuel
14 minute interview with Houston TV reporter.
She’s a warrior, all right! Worth your time!
I would like to see some data, but lots of other doctors report the same results, and I’d like to see some of their patient information, too. (Ages, other meds, vitals, timing, symptoms.)
She does say wear a mask if you can’t be on prophylaxis and to make other people comfortable. I would call her regimen a “treatment” rather than a “cure.”
But the biggest fuss has been about Dr. Immanuel’s religious beliefs. I’ve heard Baptist, Assembly of God, even Church of Christ preachers say much the same about the hidden powers in the world. Maybe not the origins, but their existence and, as Jesus Himself said, the need for prayer and fasting to deal with them.
I’ve been told that her religious views are a distraction and counter-productive for the Medical issues and “science.” But Dr. Immanuel doesn’t even bring up her religion until she’s questioned in this interview and didn’t bring it up at all in DC.
The detractors don’t understand the cultural background and how many Christians – across the spectrum from those who believe in the indwelling of the Holy Spirit to those who only remember the story of St. Michael – will recognize the theme.
COVID-19 Treatment – Analysis of 65 global studies showing high effectiveness for early treatment
https://c19study.com/?fbclid=IwAR2QTfcqe3nlW81BG8rE7pgxyUMgMlcPC2J7Un3xDTT2mqsazlHTzJurpFc
39 of the studies were peer-reviewed.
Right to Life, COVID, 16 May, 2020
The “Right to Life” means the negative right not to be killed by intentional acts. It’s not the right to force others to invest our life, liberty or property other than the duty to intervene against infringement. This is a basic negative right, not a positive right.
There’s a huge difference between personal responsibility in avoiding a risk to yourself and actively causing harm to someone else. Self-defense rather than selfish demands, using only appropriate force on others.
You know, the old “your right to swing your fist ends at my nose!” (Especially Appropriate in this case.)
*You* take the actions *you* believe are responsible. Only frequent places/businesses that require masks if you want, do the work necessary to maintain the social distancing you are comfortable with. Don’t force everyone else to do your work for you.
Front lines in the ICU with COVID-19
Reality is teaching a hard reality lesson with COVID-19.
This video concerns the minority of COVID-19 patients who require intensive care and the less than 1 percent who die of the disease. The discussion about the course of the disease and treatment is possibly too technical and brutal for the general public, so watch the whole thing with care.
However, I’m hoping to spur conversations about end of life in light of the broader COVID-19 crisis and specific crisis events.
This is a tough, highly technical discussion between Dr. Zubin Damania, a blogger otherwise known as “ZDoggMD” and Barbara McClean, MN, RN, CCRN, NP-PC, an expert in Critical Care & Intensive Care medicine in an Atlanta, Georgia teaching hospital with over 100 ICU beds. The first few minutes show Barbara McClean as a compassionate caring practitioner and educator. I believe and trust what she says about the worst case (stressing, again: fortunately these are the minority!) outcomes with COVID-19.
If you want to get to the meat of the video, there’s a “philosophical discussion” about the very real, unique in this modern age, futility of CPR in COVID-19 patients whose hearts stop due to the disease at 35:00 to 41:00.
There’s also interesting information about Personal Protective Equipment (PPE) difficulty (not shortage, but the physical reality) at the segment 30:00 to 35:00 minutes.
COVID-19 is, as Ms. McLean says, an unpredictable, sometimes deadly disease. Currently, patients can go from minor symptoms to death due to respiratory failure and cardiac arrest in as little as 4 hours. There is very little success to date in attempts to resuscitate patients who “code,” whose hearts stop, while in distress due to the virus.
I can’t stress enough that we need to talk, we need to make decisions among our families and to understand that this disease takes some options, some autonomy we have come to assume are our rightful “choices,” completely off the table. This disease doesn’t care what we want.
I’m unable to turn comments back on for this post. Please post comments to my Facebook page and I will try to keep up with replies. Let’s keep this on the level of philosophy and medical ethics. I will delete political criticisms.
Let’s keep this on the level of philosophy and medical ethics. I will delete political criticisms.
To kill or not to kill – or even to call it killing?
It seems that an advocate of Euthanasia and Assisted Suicide (EAS), which is legal in Canada since 2016, complained to the “The Protection of Conscience Project” administrators about their use of the word, “killing,” rather than “Medically Assisted Death” (MAD) when writing about the law. The wording of the objection exposes the potential limitations even on thoughts, much less the act of refusal, of physicians who object to participating in EAS.
(*EDITED An earlier version stated that licences were at risk. Not yet.
BBN 11 February 2020 12:30 AM)
More thoughts on Texas Advance Directive Act
I was asked about the #BabyTinslee case and what we should do, what can we do, in the disputed cases.
We need to educate more. People don’t understand basic medical ethics in this day of “choice.”
Autonomy doesn’t supersede nonmaleficience. In other words, the First Principle of medicine, “Cure when possible, but first do no harm,” always should guide us, rather than “wants” or “choice.”
In the end, doctors are the ones actually performing the acts and we’re most likely to understand the projected outcome. We benefit from oversight by colleagues and the community, both informally and in the process prescribed by the Texas Advance Directives Act.
Some people demand that every one of these cases go to court, for “due process” and “cross examination.”
But judges and courts can’t be as knowledgeable as doctors are. Their decisions are necessarily informed by dueling (paid) lawyers and (hired) medical experts.
In all the cases that have gone to court, the family has had quite a lot of notice, but the 48 hour notice before the committee meeting is perceived as too abrupt, especially since the relationships all appear to be adversarial by that point.
(And who could get your family to a meeting in 2 days?)
The 10 days isn’t thought to be long enough to arrange a transfer, either. Again, in many of the Court cases, the attempts to find another doctor willing to accept the patient’s care has begun before the committee meeting.
Doctors acknowledge the great trust and privileges we are given by agreeing not to abandon our patients. When we have a disagreement with a patient or surrogates (usually a familymember), we accept that we must continue treatment for a period of time. But not indefinitely.
If we could get the reforms that have been attempted to lengthen the statutory timeframe (multiple times) since before 2005, the TADA would be much better. It’s still the best process we have, currently.
Miracles in a predictable universe
We are blessed with a universe that’s predictable and testable, yet we pray for miracles. And we pray for miracles, but act as though human actions can block them. Is the will of the Creator Who spoke the physical laws into existence limited by humans if they act as though the universe is predictable and testable?
Those of us who practice medicine are limited by the physical laws, the predictable and testable, with an emphasis on the tested. Our education and experience is based on these tested predictions and guide our decisions, and we’re watched and sometimes redirected by our colleagues, patients, laws and the community.
And then, there’s the best test of all: time.
In fact, I once noted that a patient who outlived the “10 Day Rule” might have proved the doctor (who instigated the process from the Texas Advanced Directive Act) wrong. There might have been a few cases like this, just as I believe there have been miracles.
However, can you tell me how to measure these events and predict their occurrences, much less practice medicine based on them?
In the majority of TADA cases when treatments weren’t withdrawn, the patient died in the exact manner the doctors predicted, after the same interventions -and sometimes more invasive and tortuous “treatments” than the ones the doctor originally objected to.
Doing to, not for (Baby Tinslee & TADA)
“We’re doing things to her. Not for her.” (Wini King, spokesperson for Cook’s Children’s Hospital, January 3, 2020) This may be the best description of a very sad case.
Tinslee Lewis was born prematurely on February 1, 2019, with severe heart and lung defects. She had cardiogenic shock and was admitted to the Cardiac ICU at Cook’s Children’s Hospital immediately. ♡(See Cardiac Pathology ♡below.)
Even after three open heart surgeries, a fourth to close her sternum, a short time on ECMO (essentially, heart-lung bypass) and constant ventilator since July, of 2019, Tinslee’s enlarged heart and small, damaged lungs can’t keep up with the necessary blood circulation and exchange of oxygen and carbon dioxide, even with the assistance of multiple blood pressure medicines, diuretics and the ventilator on high, except when she’s still and quiet with the help of sedating and paralyzing drugs.
In response to a lawsuit against Cook’s Children’s Hospital, where Tinslee has been in the CICU since birth, Tinslee’s medical records were submitted to the Court. I’ve been able to review approximately 200 pages that are now public record, describing the constant, repetitive interventions necessary to keep Tinslee alive on the ventilator.
Tinslee’s doctors (and, the notes show, the nurses and staff) believe that they are being forced to cause Tinslee pain and suffering, while keeping her paralyzed and sedated. They report increasing difficulty with managing the ventilator so that her damaged heart & lungs can maintain oxygenation. She requires repetitive heart, lung and blood tests to guide adjustment of meds & treatments and has had several infections requiring treatment. In contrast to my earlier presumption, the notes in the records show that the ventilator and all its required meds and manipulations are indeed causing undesired problems, including fluid overload, infections and cardiopulmonary distress, in addition to her underlying lung disease. Even the baby’s growth, something we usually celebrate, increases her risk of cardiopulmonary insufficiency.
Those records also contain notes from many attempts to explain and council Trinity Lewis, Tinslee’s mother, about her baby’s underlying problems and prognosis and the reasoning behind, in contrast to some past media reports.
Ignoring the fact that doctors, not hospitals, practice medicine in Texas, Texas Right to Life Lawyer Joe Nixon is quoted, claiming that the “hospital ” has decided to withdraw treatment. Texas Attorney General, Ken Paxton, is shown to have Tweeted that the problem is a “legal issue,” rather than an ethics and justice matter of forcing doctors (and by their orders, nurses and other staff) to cause pain and suffering for a little girl who is dying as her body fails to heal, in spite of every intervention possible.
Many people, out of compassion, object that “the family ” should decide when to withdraw life support. Yet, the family members aren’t watching the oxygen levels drop while they rinse Tinslee’s airways with a bicarbonate solution to keep her lungs clear. And it’s certainly not the lawyers that are probing, injecting, measuring and adjusting constant, innumerable hourly interventions done to a baby who must be sedated and paralyzed to prevent cardiac and respiratory distress.
In spite of the diligent complicated interventions and care of the doctors and nurses at Cook’s, there have been comments in blogs and social media that the “hospital” wants to “kill” Tinslee. Startlingly, AG Paxton called the latest Court ordered, indefinite hold on removal of life support a “Stay,” as though the doctors, not her multiple medical problems, would kill Tinslee. He also misrepresents the process that Cook’s Children’s Hospital and Tinslee’s doctors followed,
“The statute fails to require that physicians provide an explanation of why they refused life-sustaining treatment and provide the patient’s family with adequate notice and opportunity to argue their position prior to the committee reaching a decision, effectively allowing the government to deny an individual’s right to his or her own life and to do so without due process.”
In fact, though, it is the lawyers, particularly at Texas Right to Life, who are turning a little girl’s tragedy into a continuation of their legal battle against the Texas Advance Directive Act. I’ve covered the benefits of and the struggle to improve the Act – repeatedly blocked by TRTL and their lawyers – for years on both WingRight.org and Lifeethics.org
The Act, TADA, was hammered out in 1999 by a group of stakeholders including patient and disability advocates, hospitals, doctors, ethicists and lawyers. Texas’ prolife organizations, including TRTL and the organization for which I served on the Board of Directors for 15 years, Texas Alliance for Life, and for whom I wrote this essay.
Briefly, TADA allows a balance and legal options when there’s a difference in opinion between a patient’s desire for a given treatment and the medical judgment (a combination of education, experience, and the standard of care) of the doctors who are tasked with the most difficult medical and surgical cases.
I’ll admit that it’s my opinion – and only my opinion – that the lawyers hate that TADA provides a safe haven from lawsuits if doctors follow the law (!). I slowly came to this conclusion over the years because at virtually every Legislative hearing and stakeholders’ meeting about any changes to the Act, the lawyers bemoan the fact that doctors don’t have to go to court over each of these cases and that they face no legal penalty or “liability.”
Poor Tinslee Lewis will most likely never leave the hospital alive. Disease and death don’t respect “due process,” but, they are predictable and an inevitable part of life. Hopefully, we will see her mother and those who love her come to find peace with her death, celebrating the time they’ve had to be with her, especially these last 2 months. However, I fear that the lawsuits will continue for years, adding to their grief.
Edited 1/19/2020 for a typographical error: in the secondparagraph, “cardiogenic” replaced “carcinogenic.” BBN
♡Ebstein Anomaly – Cardiac Pathology 101, about as simple as I can make it (and understand, too);
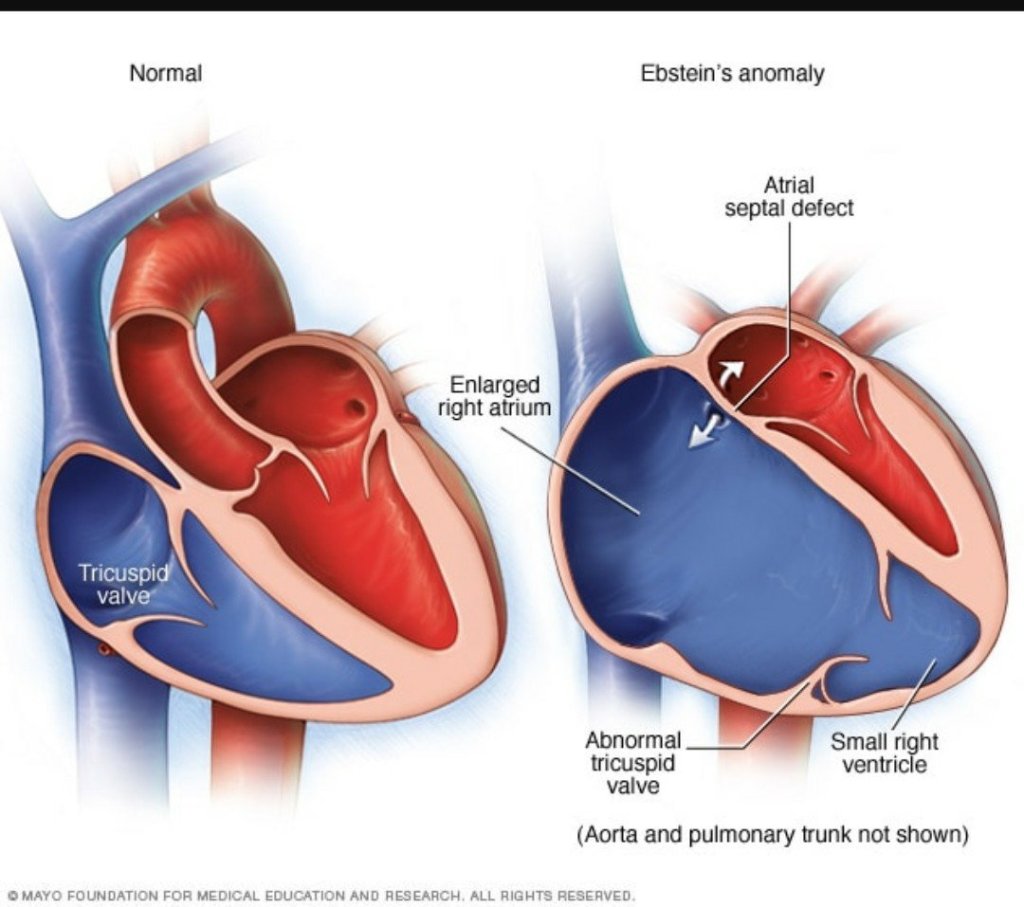
(Thanks to Mayo Clinic)
Babies born with Ebstein Anomaly have a malformed right and atrium and ventricle and misplaced (tricuspid) valves between the right sided ventricle and atrium. The larger right ventricle can’t pump efficiently.
In addition, the blood the right ventricle tries to pump into the lungs leaks/flows/churns (risking blood clots) back into the right atrium, which grows even bigger, with even thicker walls. The ventricle also grows bigger. When the muscle fibers of the chamber walls get stretched apart enough, they are less inefficient. (Think of two hands gripping at the fingers. The farther out the grip, palm > 1st joint > fingertips, the less strength and pull on the opposite hand.) (For the geeks: Frank-Starling law.
The lungs aren’t efficiently filled with blood, they don’t expand, the pressure builds up in them and efficient exchange of gasses doesn’t take place.
In the meantime, the blood backs up in the body, the liver, kidneys and extremities & eventually the left side of the heart, which can hypertrophy , too.
The enlarged heart puts pressure on the lungs and nearby soft tissue, including the blood vessels coming to the heart.
The combination of leaking high pressure blood vessels and the body’s increasing fluid in order to try to pump what oxygen there is, leads to edema or swelling of the body.
Sometimes, the fetal atrial-septal defect stays open, allowing mixing of the un-oxygenated blood from the right, with the oxygenated blood. This malfunction can help, temporarily.
With the high pressure, poor flow, and actual physical damage due to the mass of the heart, none of the organs can function well. Increased activity, stress, and growth will increase the demand for oxygen, kidney & lung function.
Experimental Abortion – Schrodinger’s Fetus
What ethics review board approved a randomised trial to temporarily prevent the ending of the life of a human embryo or fetus, with a planned surgical abortion as an end point?
Horrifying report about human experimentation: Obstetricians at the University of Southern California have announced that they stopped a study using progesterone to reverse the anti-progesterone effects of mifepristone in medical abortions.
According to the NPR:
“For the study, the researchers aimed to enroll 40 women who were scheduled to have surgical abortions. Before their surgical procedures, the women received mifepristone, the first pill in the two-medication regimen that’s used for medical abortions. The women were then randomly assigned to receive either a placebo or progesterone, which advocates claim can block the effects of mifepristone.“
Ignore the fact that only 12 women signed up over 6 months, that in spite if the claims if the researchers, the mifepristone was the actual, immediate cause of the complications that included 3 women needing ambulance transport to a hospital for excessive vaginal bleeding and 2 others dropping out due to some other side effects.
But you should certainly – they hope – forget that 4 of the babies exposed to progesterone and 2 who received placebo after the mifepristone continued to live for 2 weeks until their death at the hands of an Obstetrical surgeon. That’s half of the study group!
There’s no question that I consider it unethical to cause the intentional, interventional death of any human who isn’t a threat to life for another. It’s heinous that our laws allow the best medical technology in the world to kill members of our species, because they aren’t considered human-enough to possess the inalienable human right not to be killed.
But there’s an additional ethics problem in this case: a strong “yuck factor” (aversion) to the idea of purposefully experimenting with ¢ lives of humans, both the mother and her child, planning to monitor the signs of the prenatal human’s life, anticipating his or her death by surgical abortion.
Half of the original mothers had planned two weeks (14-16 days)delay with serial ultrasounds, confirming her baby’s heartbeat. (Remember this experimental protocol the next time an abortion advocate complains about State-mandated waiting periods and pre-abortion ultrasounds.)
Let me repeat: half of the nascent human beings experimented upon/ lived two additional weeks after exposure to the mifepristone poisoning. Only one of the 12 pregnancies resulted in what would be considered a “normal” medical abortion.
Eventually however, all of them were finaly “terminated.” After two weeks of observation – Schrodinger’s humans.
Note: Due to some sort of technical problem at the website, I wasn’t able to purchase the article, so this is based on the abstract and NPR report.
Edit 12/9/19, BBN: I was able to purchase access to the article (24 hours for $60!). There’s no change in the facts other than to note that the authors report continued life of the prenatal humans as 6 of 10 subjects: 4 of 5 who finished the trial and received progesterone, and 2 of 5 who were randomized to the placebo arm.
Parachutes don’t save lives?
Not when the jumper starts only 2 meters from the ground.

“Parachute use to prevent death and major trauma when jumping from aircraft: randomized controlled trial
BMJ 2018; 363
“”Ah, but the method of madness matters! The non-participating passengers flew at 800 km/hr at an altitude of 9,146 m, but the trial participants jumped a whopping 0.6 meter (2 feet) from a plane traveling at an incredible 0 km/hr. The authors point out their trial’s glaring limitation — an inability to generalize to higher altitude jumps — and use it make a point that health journalists would be wise to remember:
“When beliefs regarding the effectiveness of an intervention exist in the community, randomized trials might selectively enroll individuals with a lower perceived likelihood of benefit, thus diminishing the applicability of the results to clinical practice.
This study was conducted in response to a Christmas, 2003 BMJ article decrying the lack of RCT (Random Controlled Trials) for the efficacy of parachutes. As the authors of this article point out, even RCT’s have their limits.
As one review explains,
Put plainly, if most people already think an intervention works, then an RCT may end up with enough bias in its design that the conclusion ends up clinically meaningless. Sometimes, an RCT is truly unethical, and other times an RCT really might be needed to test an intervention taken for granted. Health journalists should scrutinize an RCT’s methods closely.
I’ve disabled comments on the blog. Please leave your comments on my Facebook page, “Beverly Nuckols.”
Cook’s Children’s Press Release on Tinslee Lewis
The Press Release is published in .pdf on the hospital’s website. Here’s the text:
Cook Children’s Statement Regarding Patient Tinslee Lewis Fort Worth, Texas (November 10, 2019) –
Tinslee Lewis is a beautiful baby who has captured the hearts of many at Cook Children’s since her premature birth nine months ago. She was born with a rare heart defect called an Ebstein’s anomaly and has undergone several complex surgeries at Cook Children’s in an effort to improve her heart function. Further complicating matters, she also suffers from chronic lung disease and severe chronic pulmonary hypertension. Due to these complications, she has spent her entire life hospitalized in Cook Children’s intensive care unit. She has required artificial respiratory support throughout that time, and has been consistently on a ventilator since July.
In the last several months, it’s become apparent her health will never improve. Despite our best efforts, her condition is irreversible, meaning it will never be cured or eliminated. Without life-sustaining treatment, her condition is fatal. But more importantly, her physicians believe she is suffering.
To maintain the delicate balance necessary to sustain Tinslee’s life, and to prevent her from pulling out the lines that are connected to the ventilator, doctors have had to keep her constantly paralyzed and sedated. While Tinslee may sometimes appear alert and moving, her movements are the result of being weaned off of the paralyzing drugs. We believe Tinslee is reacting in pain when she’s not sedated and paralyzed.
Cook Children’s has made heroic efforts to treat Tinslee’s condition, all while being very transparent with her family regarding her poor prognosis. Despite those extraordinary efforts, Tinslee’s condition has not improved. At the request of Tinslee’s family, we have reached out to nearly 20 facilities across the country to see if any would be willing to accept Tinslee as a patient. Some of the facilities include:
Texas Children’s Children’s Memorial Hermann Hospital Dell Children’s Dallas Children’s Medical City Dallas Children’s Medical Center Oklahoma City Children’s Hospital of Atlanta St. Louis Children’s Children’s Hospital of Philadelphia Johns Hopkins Methodist Hospital San Antonio University Hospital San Antonio Boston Children’s Children’s Hospital of Los Angeles Arkansas Children’s C.S. Mott Children’s Michigan LeBonheur Children’s Memphis Rady Children’s Children’s Hospital San Antonio CHRISTUS
All have said our assessment is correct and they feel there is nothing more they can provide to help improve this precious child’s life.
A team of Cook Children’s doctors nurses and staff have given their all to help Tinslee. While, we believe every child’s life is sacred, we also believe that no child should be sentenced to a life of pain. Removing this beautiful child from mechanical ventilation is a gutwrenching decision for Cook Children’s physicians and staff, however we feel it is in her best interest to free her from artificial, medical intervention and suffering.
Winifred King
Assistant Vice President of Public Relations Cook Children’s Health Care System
Baby Tinslee Lewis and the Texas Advance Directive Act
I was a relieved to hear that the doctors caring for 9 month old Tinslee Lewis decided not to remove her ventilator on Sunday, November 10, 2019. Their decision, most likely due to public outcry, was announced 2 hours before removal was planned. Later in the day, and a local judge issued a restraining order that mandates continuing the ventilator until at least November 22 unless an appropriate transfer to another facility can be arranged.
At first glance, this sounds like several other stories about disputes between the family of a patient and medical professionals who have invoked the provision in the Texas Advance Directives Act(TADA) that allows for removal of life sustaining treatment. However, from what I’ve read and the hospital’s statement, I’m concerned that this time the law may have been invoked based on “quality of life” rather than the futility of the treatment and the suffering it causes.
(Note: I want to be very careful to point out my limits. The following medical and legal information about this case comes from what I’ve gleaned from Facebook, blogs and Twitter posts, as well as a few news articles like this one. I’ve tried to be as factual and accurate as possible. It’s important to understand that I don’t know all the details and that any conclusions I draw are merely my opinion.)
Tinslee has lived her whole life in the ICU at Fort Worth Cook’s Children’s Hospital. She was premature and was diagnosed with a congenital heart defect, Epstein’s anomaly, that in spite of several surgeries led to heart failure and caused her heart to become so enlarged that it damaged her lungs. She’s been on a ventilator since July.
Her doctor or doctors reportedly believe that Tinslee is in pain and suffering. In order to keep her comfortable and to prevent her pulling the ventilator and feeding tubes, they must use paralyzing drugs and sedation. An attending doctor responsible for Tinslee’s care invoked TADA and a hospital committee agreed that the continued use of the ventilator is inappropriate. On October 31, the family was notified that the ventilator would be discontinued at 5 PM on November 10.
I became concerned when I saw the video posted at Texas Right to Life, showing a beautiful girl with apparently healthy skin, reacting to voice and touch. In the video, she doesn’t move her right leg, barely opens eyes and only seems to point her eyes to lower right. Still, the treatments, including sedation, seem to be working and she doesn’t appear to be in distress or pain.
A hospital spokesperson, Winifred King, assistant vice president of public relations for Cook Children’s Health Care System, sent out a statement by email, that is quoted in part by the Fort Worth Star Telegram:
“In the last several months, it’s become apparent her health will never improve,” King said in a statement via email. “Despite our best efforts, her condition is irreversible, meaning it will never be cured or eliminated. Without life-sustaining treatment, her condition is fatal. But more importantly, her physicians believe she is suffering.”
And,
“While we believe every child’s life is sacred, we also believe that no child should be sentenced to a life of pain,” said Winifred King, assistant vice president of public relations for Cook Children’s Health Care System, in a statement. “Removing this beautiful child from mechanical ventilation is a gut-wrenching decision for Cook Children’s physicians and staff; however, we feel it is in her best interest to free her from artificial, medical intervention and suffering.”
(Kaley Johnson, Fort Worth Star Telegram https://www.star-telegram.com/news/local/fort-worth/article237223826.html accessed 11/10/19)
Hesitantly, I find myself second guessing the decision of Tinslee’s doctor(s) to invoke TADA and of the hospital ethics committee to affirm that the ventilator is inappropriate medical care. As I wrote above, I can’t know the real medical circumstances and certainly haven’t examined Tinslee or even read her chart. I’m not a pediatric cardiologist or pulmonologist and may not understand her prognosis as she grows and develops. Has she required chest tubes because of the ventilator? Is she growing? Will a larger body put too much strain on her heart or will growth allow time – and room – for her lungs to heal? Will she be able to have a tracheostomy and would it make her care easier and her more comfortable?
However, there’s no sign that the ventilator itself is causing damage to her lungs and there is evidence that the medication helps Tinslee tolerate the mechanical intervention.
The wording of Ms. King’s statement makes it appear that the doctor(s) decided to end the ventilator treatment based on a perception of her quality of life, rather than on their knowledge of the futility of the treatment and the damage it causes. In my opinion, “quality of life” is a very personal value judgement. As I’ve noted before,
“Although no reason is required by law, in every case I know of the doctor has made it clear that the requested treatment is causing suffering and/or actual harm and violates the First Principle: “Cure when possible, but first, do no harm.”’
The good news is that TADA allows, and Tinslee’s family were able to, access practical and legal assistance.
Ms. King shared a list of 19 hospitals that, as required by TADA, the hospital administration has contacted in an attempt to find other doctors and facilities that will accept Tinslee as a patient. All refused the transfer, apparently agreeing with Tinslee’s doctor (and casting doubt on my conclusion).
TADA also allows the family to seek a delay through the local courts. Texas Right to Life helped Tinslee’s family by providing a lawyer and legal advice. They also sent out a plea on Friday, November 8, asking the public to call and email Cook’s administrators about Tinslee. Several State legislators have also become involved.
Now, Tinslee’s mother and family and the hospital will have another 12 days to try to find someone willing and able to treat her.
Questions still remain: Is there any long term facility that is able to offer the ventilator and sedation that Tinslee needs? Or must Tinslee live sedated and paralyzed in the ICU for the rest of her life?
But there shouldn’t be any question weighing whether Tinslee’s “quality of life” is worth living.
Texas transgender (7 yo) case
I don’t believe it’s appropriate for a child to undergo transition at such an early age, but there’s a few gaps in this story.
There is very little media coverage of the case, with opinion from only one side published online. I picked the report about the court decision that’s most comprehensive, even with some errors.
Mostly, this appears to be an especially ugly divorce battle. The dispute about transition has been going on since the child was 3 years old.
The child is one of two twins conceived by in vitro fertilization using the father’s sperm and a donor egg. The mother carried the two to term and delivered.
The mother filed the suit to end joint custody, but the father demanded that the jury decide custody, rather than the judge.
The jury was charged with 2 questions: should one parent have sole custody and should that parent be Mr Younger. They answered yes and no: one should have sole custody, but it shouldn’t be the father. The judge will rule this week on who gets custody & conditions.
I’m not sure, but I’m reading that there’s no immediate plans for puberty blockers & finding quite a bit of info that the blockers aren’t permanent.
I can’t help but hope there’s more to this story, because I still can’t accept a decision like this, at this age.
Entire abnormal human genome in vaccine?
Quintessential anti-vaccine propaganda. The first sentence indicts the source, Mike Adams, the founder of “Natural News” and seller of food supplements like Organic Broccoli Sprout Capsules with a side of conspiracy.
Yet, that’s what they accuse the “cancer industry” of doing.
Finally, the accusations in the video have been rejected in court. This, in spite of the low requirements for vaccine injury compensation.
Edit 10:15 AM 10/07/2019: The MMR assay report from Corvelva is here. I’m skeptical about the “entire genome” supposedly found. Are they saying that all 23 chromosome pairs are present in each dose? BBN
Vacationing for health
It’s good to have confirmation.

But jobs that don’t allow vacation probably have different effects than jobs that do allow time off.
Arguing Abortion on YouTube
I usually agree with this doctor. But not about abortion. ZDoggMD, Zubin Damania, has a sense of humor and a sense of balance. But today, he demands that we to “come to the center” because 1 in 4 women in the US have an abortion by age 45. “It happens.”
Well, according to the 1860 US Census, approximately 25% of families owned slaves. “It happen(ed).” Common ground was hard to find there, too.
The question is whether or not abortion ends the life of a human that is human-enough to possess the Human Right not to be killed. Are they one of us and can we kill them if they don’t threaten our lives?
The first question has been definitively answered, at least scientifically. Louise Brown was born 5 years after Roe v Wade. Serial ultrasounds showing the progression of the egg to embryonic organism to fetus were possible soon after. (I’m tempted to echo the ZDogg, “Grow up and get into the 21st Century.” But of course, I won’t.)
Answering these questions according to ethics and law can’t be addressed by science and requires a bit more discussion. Nevertheless, the trend in Western societies has been toward including all humans as rights bearers endowed with at least the right not to be killed or treated as the property of another and preventing legally sanctioned killing and enslavement, regardless of characteristics, abilities, or background.
Beyond the life of the mother, the rest of ZDogg’s arguments are the usual justification for what I call, “I want” ethics, including arguments for the “control of the woman’s body,” the health of the woman, and exceptions for rape and incest.
Nik Hoot, a 20 year old young man from Indiana, lost his feet and part of his legs and fingers to an attempted abortion, but survived to be adopted, eventually a State Semi Finals high school wrestler, and a productive member of society. His mother’s body didn’t lose limbs; his did. As he says, he has to “live with someone else’s choice.”
As to the health of the mother, how could anyone know at 12 weeks that there will be sequelae at or after delivery?
The safety of abortion is most often reported using short term data. There’s support for increased mortality and morbidity in the long term, however.
Late discovery of fetal abnormalities isn’t a good argument in favor of induced abortion, either. After 15 weeks and definitely after 20, it’s statically safer for the mother to carry to term.
I won’t even entertain arguments that crime is down because the unwanted are killed. “Minority Report” has a double meaning, here.
Let’s face it: the wrong human is killed by abortion justified by reason of rape or incest. If you cringe at that statement, you might want to consider why.
Beverly B Nuckols, MD
Updated information on TRTL, end of life, and money
One Texas Right to Life (TRTL) lawyer has posted an update on Facebook about the “rescue” of Mrs Carolyn Jones. I’m afraid that, as with the declaration that another patient was “slain,” TRTL is gaming the Medicare funding and Texas medical systems for political purposes.
Emily Cook, General Council for TRTL, wrote that she worried that “funny business clinically would happen as we moved her” from the hospital where Mrs. Jones has been admitted for over 6 months, where the docs had weaned her off the ventilator and wanted her to transfer to a more appropriate level of care facility over 2 months ago.
Emily says TRTL spent their own money (*see my last paragraph) to put her in a private ambulance and take Mrs. Jones to another hospital ER. That hospital couldn’t provide dialysis, so they in turn transferred her via ambulance somewhere else, to yet another hospital until admission can be arranged at the nursing home.
Cook-ing the system
Mrs. Jones’ Medicare funding for the original hospitalization is bound to have run out some time ago. Normally, Medicare will allow 90 days per admission, with an extra 60 “reserve” days, once per person, per lifetime. The patient is responsible for part of the bill from the first day of admission, and for the total hospital costs after the eligible days.
But there are still Medicare regulations to deal with in the case of “Medicare eligible” patients, even when they aren’t paying.
Medicare makes it very difficult and risky for everyone to navigate the private pay process. When I had a question in my private medical office about whether Medicare would cover something, we had the patient sign an informed consent agreement and an acknowledgement that the patient might have to eventually pay if Medicare denied the service. Then we performed the service, filed the charge with Medicare, waited to be denied, and then tried to Bill the patient. I gave away a lot tetanus vaccines and removed a lot of moles and warts for free to avoid the risk of “fraud and abuse” from the likes of Janet Reno.
The same risk would have applied if the hospital had privately charged Mrs. Jones’ Dialysis.
I don’t believe the first new hospital is at risk for a charge of “dumping” if they documented a legitimate reason. However, both new hospitals will be able to charge the Jones copays and co-insurance. They may also find Medicare coverage limited because of the way Mrs. Jones left the original.
“Medicaid limits 2019” (a .PDF)
I certainly don’t know the Jones’ financial circumstances, and I may have over estimated the maximum income in early speculation. However, there are strict maximum Medicaid income and asset levels. These vary according to age, disability, and marital status. (Even the government bureaucratic Leviathan doesn’t want the spouse if a nursing home patient to end up indigent.)
In my experience, the social workers and benefits experts at hospitals and nursing homes are experts at negotiating and translating the bureaucracy. In addition, the disabled Medicare eligible person will have access to a benefits specialist. I’ve never had a hospital discharge and nursing home admission blocked by this “paperwork.” Certainly not for months at a time.
I hope TRTL assists the Jones family with what is certain to be several enormous hospital bills. As long as they pay the bills directly, the funds won’t be counted as income to Mrs. Jones.
Why does TRTL lie? (UPDATE)

they now post that a woman, Mrs. Carolyn Jones, had to be “rescued” from hers, “racing” to another facility “in the middle of the night.”
The family were given notice that they needed to transfer Mrs. Jones in March. They’ve had another doctor and three facilities capable of providing the treatments she needs waiting to accept Mrs. Jones.

And now, TRTL – in direct competition with – and with absolutely no mention of – Mrs. Jones’ family’s GoFundMe campaign – has been raising money in Mrs. Jones’ name. They state that the funds will be used for (TRTL) lawyer’s fees in addition to Mrs. Jones’ healthcare needs and that “excess” funds will go to help (TRTL’S) efforts for other patients.
I hope that TRTL’s money will also be used to pay for the very large hospital and doctor’s bills that the Jones family will receive. While there’s a chance that Texas Medicaid will pay for three months of medical bills, retroactively, Medicare doesn’t pay for hospitalizations over 90 days and has a 20% co-insurance (co-pay).
That’s bound to have added up in over 6 months.
We’ll just have to trust that TRTL won’t lie again.
Edit, Updated information:
One of the bloggers has told us more about that “rescue.” (Or today’s story, anyway.)
TRTL put her in a private ambulance and took her to *another ER,* one that couldn’t provide dialysis, so they then transferred her somewhere else.
There were comments about the first Hospital refusing transfer — no, refusing to be complicit with “dumping” a patient. Discharging to without ( or even with) acceptance of the transfer from the docs at the other facility is highly irregular and likely illegal.
Much has been said about funding. Yes. It appears that Medicare funding ran out, so no longer paying. 90 days per admission, with an extra 60 days over, under certain conditions.
About that Medicaid funding: I don’t know the limits of the mandatory asset tests, but the yearly income level is $60,000. One way to adapt is to spend money on medical costs.
Medicare makes it difficult to navigate the private pay process. When we had some question, we got informed consent, promise to pay, then performed the service, filed with Medicare, waited to be denied, then tried to Bill the patient. The risk is always a charge of “fraud and abuse.”
The same thing would have happened if the hospital had privately charged for Dialysis.
(5/20/19, BBN)
False story about Texas Advance Directives Act (TADA)
Mrs. Jones is not dependent on the ventilator.
In fact, it sounds like Mrs. Jones has had excellent treatment at the hospital,
Mr. Jones told the Texas Senate Health and Human Services Committee that the doctors at the hospital successfully weaned Mrs. Jones from the ventilator.
He also said that three other facilities are ready for her admission.
I’m happy to see that today’s article by reporter Tony Guajardo quotes both opponents and supporters of TADA and corrected the impression that Mrs Jones is dependent on the ventilator: “She requires dialysis, occasionally needs a ventilator for breathing assistance, and uses a feeding tube.“
And yet, today’s The Texan article still misrepresents this case: “UPDATE: Recovering Beaumont Woman’s Life-Sustaining Treatment to End Due to 10-Day Rule.”
There’s also a quote from Mrs. Jones’ daughter, repeated from the earlier article: ““My mom is going to die on Monday because of a law that saves hospitals money.”
It turns out that money and Medicaid paperwork is actually what is keeping the family from allowing Mrs. Jones to be transferred to another doctor and facility. The family is concerned that they (rather than the hospital) will be responsible for the costs of Mrs. Jones’ care.
This is in spite of the fact that when a patient first goes on dialysis, she becomes immediately and automatically eligible to apply for Medicare and Social Security Disability.
Depending on assets and income, patients unable to work on dialysis also qualify for Medicaid and other State benefits in Texas. Medicaid will even pay bills retroactively for three months.
The good news is that she isn’t dependent on the ventilator, dialysis is not constant but only 2-3 times per week and paid by Medicare, food and water by the feeding tube can’t be withheld under TADA.
Hopefully, the Jones family will finally agree to transfer her, even if costs them more than her Medicare & Social Security Disability will pay.